Not too long after he started working in academic medicine, Robert W. Gereau IV — then on the faculty at Baylor College of Medicine in Houston — accepted an invitation to lecture about his work to doctors and scientists at the Washington University Pain Center.
His research and training involved cellular changes in the brain in response to experience — how people learn and adapt to the environment.
“We looked at plasticity and memory and learning, and coming from that context, I began to think of chronic pain as a way that the brain’s plasticity could become maladaptive,” Gereau recalled. “We had made what I thought were some interesting discoveries about how tissue inflammation could lead to hypersensitivity to heat. For example, when you get a sunburn, if you use warm water to wash your hands or take a shower, you tend to experience pain because your sunburned skin is very sensitive to heat.”
From that observation, Gereau’s lab began to zero in on how heat-sensitive signals are transmitted and what ion channels in cells carry those signals. He was searching for new ways to treat the problem of heat hypersensitivity by uncovering the cellular mechanisms that create the problem. Those were the findings he presented in that initial lecture at Washington University.
He remembers being surprised by the number of white coats in attendance that day. He was accustomed to addressing bench scientists at his lectures, but a number of physicians from the School of Medicine were in the room, too. One of them spoke with Gereau after the talk.
“He said something like, ‘That’s really impressive work you guys have done, but, of course, it’s meaningless for our patients,’” Gereau recalled.
“I asked what he meant, and I told him about sunburn and warm water. And he said, ‘Yeah, but that’s not really a clinical problem. You can solve it by lowering the water temperature in the shower.’”
Gereau recalls that conversation as his Eureka moment.
“I was a little hurt at first, but as I thought about having worked so hard on a problem that wasn’t really a problem, it illustrated the importance of basic scientists and clinicians talking to each other,” Gereau said. “If I was going to conduct research on pain, I needed to try to do it in ways that would help patients.”
He has come a long way since.
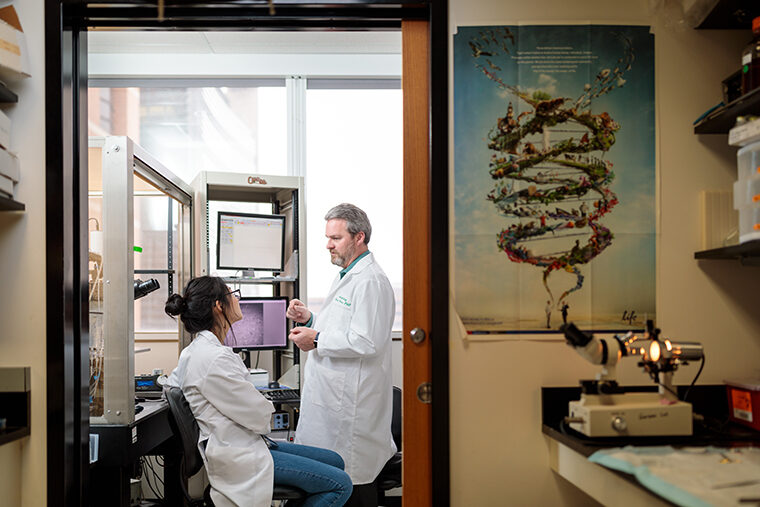
Treating pain with light
Not long after that lecture in 2003, Gereau was offered a faculty position in the Department of Anesthesiology. He’s been at Washington University ever since and is now the Dr. Seymour and Rose T. Brown Professor of Anesthesiology, director of the Pain Center and chief of basic research in anesthesiology. Much of his work involves helping guide basic researchers and clinicians who specialize in treating pain.
“I talked to my clinician colleagues about how it could work to have a nonclinician heading the Pain Center, and they were very receptive,” said Gereau, also a professor of neuroscience. “It works well because of the collaborative culture here, which is why I was so excited to join the faculty. Interaction between physicians and scientists is what makes Washington U unique and what makes my job so rewarding, because all of us are focused on helping patients.”