In the delivery room, circumstances can turn dire on a dime if the patient starts losing excessive amounts of blood. One minute she seems fine, and the next, vital signs plummet, the patient crashes, and the care team may need to scramble for a blood transfusion or perform surgery.
All too often, that alert may arrive too late. Postpartum hemorrhage is the leading cause of maternal death worldwide. Patients themselves may not notice, and there are few ways to easily measure the blood pouring out (or pooling in the uterus) during delivery. Even the most eagle-eyed doctor or nurse cannot accurately estimate blood loss from visual indicators alone.
Modern medical sensors have limits, said Christine O’Brien, an assistant professor of biomedical engineering at Washington University in St. Louis. Counting bloody rags or collecting blood in calibrated drapes may seem simplistic, but such techniques remain among the few ways to warn of excessive blood loss. A more accurate and continuous early-warning system could potentially prevent 50-90% of those maternal deaths from hemorrhage when paired with adequate treatment, she estimated.
Blood loss is “difficult to measure and if you wait on normal vital signs like heart rate or blood pressure. Those can remain stable for up to 1,500 milliliters of blood loss,” she said. (Postpartum hemorrhage is classified as blood loss of at least 1 liter, or 1,000 milliliters, within 24 hours of birth).
Tracking drops in blood pressure also won’t necessarily provide the right data because modern delivery rooms are constantly adding medications and fluids to the patient that might affect that measurement.
Instead, O’Brien, with a five-year $2.8 million grant from the National Heart, Lung, and Blood Institute, a part of the National Institutes of Health (NIH), aims to develop a wearable device that tracks blood loss through measuring cardiovascular features from a novel light-based sensor that measures changes in hemoglobin and blood flow.
This measurement produces waveforms based on how the heart is pumping and how the rest of circulatory system resists that flow. The shape of those waveforms changes based on the state of a person’s cardiovascular system. Using statistical and machine-learning algorithms, they can determine which features of the waveforms are correlated with absolute blood loss.
With an affordable wearable device that fits on a wrist and tracks blood flow, “we’ll be able to have a much clearer signal when someone is hemorrhaging,” O’Brien said.
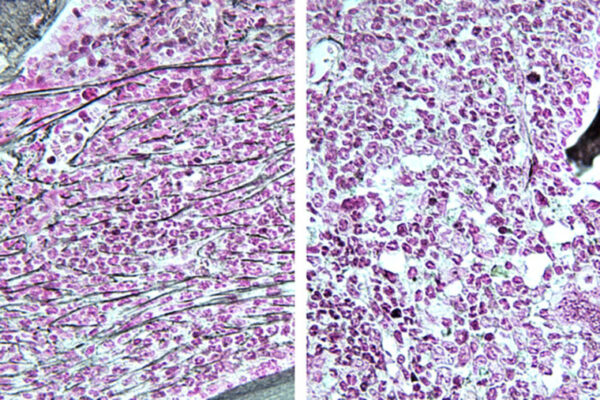
The device will be tested on animal models with differently pigmented skin to ensure skin color does not impact the sensor readout. In devices that run on light-based sensors, like pulse oximeters, skin color can affect the accuracy of the blood oxygen-level measurements. Skin tone shouldn’t impact reading of this new light-based sensor’s waveforms, but they’ll be testing it nonetheless in both preclinical models and in a diverse mix of human test subjects to ensure the sensor works correctly under differing circumstances. That also includes testing it on subjects with varying levels of hemodilution (hemoglobin being watered down by other fluids).
Though they are working on a way to track blood loss, the overarching aim is to prevent postpartum hemorrhage, O’Brien said. With early warning, oftentimes simple, low-cost interventions, such as massaging the uterus, could stop the bleeding. Not all hospitals are fully stocked to handle an emergency blood transfusion or surgery, so it’s better not to lose so much blood in the first place.
“You can find yourself in an emergency very quickly,” O’Brien said.
Originally published on the the McKelvey Engineering website