Alzheimer’s disease and frontotemporal dementia are devastating disorders that emerge following the buildup of misfolded proteins in the brain.
The newest generation of Alzheimer’s therapeutics targets accumulations of the protein amyloid beta with engineered antibodies, but the results have been underwhelming, with some adverse effects, not to mention using engineered antibodies can be prohibitively expensive.
Researchers at Washington University in St. Louis are taking a new approach, looking to design vaccines that will train a person’s own immune system to take out these accumulations of amyloid beta and tau proteins.
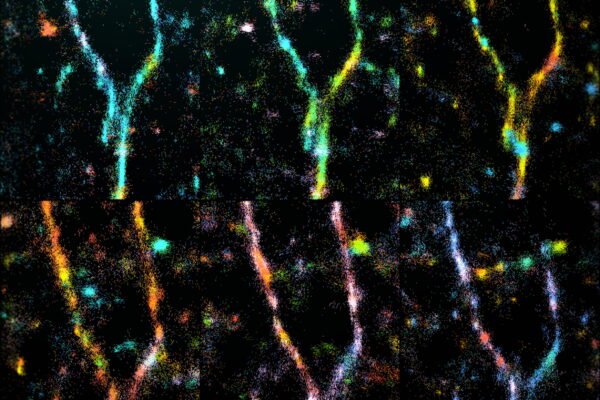
With a $2.9 million grant from the National Institute on Aging, part of the National Institutes of Health (NIH), researchers Jai Rudra, PhD, an associate professor of biomedical engineering at the McKelvey School of Engineering, and Meredith Jackrel, PhD, an associate professor of chemistry in Arts & Sciences, will design vaccines that generate anti-amyloid beta and anti-tau antibodies using Rudra’s vaccine platform of peptide nanofibers.
Key to the success of this project are vaccine designs that don’t induce inflammation as it is a constant challenge for the field to counter the chronic inflammation that comes with age.
Rudra said previous trials used strong vaccine adjuvants to ensure attacks on amyloid beta, but that caused adverse effects in some patients. Adjuvants can ensure that the immune system will see misfolded proteins as “foreign material,” but the inflammation that ensues could do more damage than it’s worth. Instead, Rudra is using a nanofiber platform he developed in previous vaccine research.
“Nanofibers have unique properties that make them attractive for making antibodies to tau and amyloid beta proteins, and they don’t cause inflammation like other adjuvants,” he said.
Jackrel noted that recent trials of dementia treatments have failed in part because of the brain inflammation that ensues, which is why they are going down a different path with nanofibers.
“The noninflammatory nature of these is a good strategy to counter that,” she said.
The nanofibers work better because amyloid beta and tau are presented on the surface of the nanofiber in such a way that the immune system will not generate as much inflammation in its wake.
Big picture
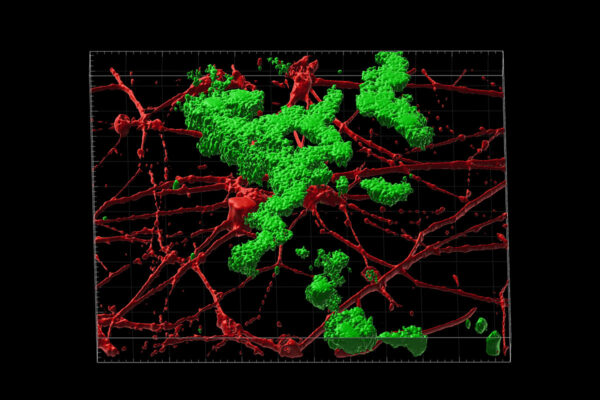
Jackrel and Rudra will work with WashU Medicine researchers to test their vaccines. Tim Miller, MD, PhD, the David Clayson Professor of Neurology, and Kathleen Schoch, PhD, an assistant professor of neurology, will assist by testing the vaccines on transgenic mice that develop disorders that mimic various dementias in the brain.
They’ll test it both as a preventive treatment and a post-symptom treatment, though Rudra expects the prophylactic use to be more effective. The problem with breaking up tau and amyloid clumps after people are symptomatic of dementia is that it may already be too late.
“Disaggregating them is going to be very challenging,” said Rudra, noting that it will likely be much easier to attempt to prevent the snowballing of dementia symptoms by nipping all that neuroinflammation in the bud, potentially as early as people are entering middle age.
This also aligns with other initiatives at WashU to develop blood tests for early detection of a variety of neurodegenerative diseases. Further projects outside biomedical engineering are looking to apply all manner of medical and lifestyle treatments beyond just immune system big guns.
Dementia and neurodegeneration are not one single disease or stem from one single source, so it will take a multipronged approach, Jackrel said.