Researchers at Washington University School of Medicine in St. Louis have developed a way to capture the effects of aging in the development of Alzheimer’s disease. They have devised a method to study aged neurons in the lab without a brain biopsy, an advancement that could contribute to a better understanding of the disease and new treatment strategies.
The scientists transformed skin cells taken from patients with late-onset Alzheimer’s disease into brain cells called neurons. Late-onset Alzheimer’s develops gradually over many decades and only starts to show symptoms at age 65 or older. For the first time, these lab-derived neurons accurately reproduced the hallmarks of this type of dementia, including the amyloid beta buildup, tau protein deposits and neuronal cell death.
By studying these cells, the researchers identified aspects of cells’ genomes — called retrotransposable elements, which change their activity as we age — in the development of late-onset Alzheimer’s disease. The findings suggest new treatment strategies targeting these factors.
The study appears Aug. 2 in the journal Science.
“Sporadic, late-onset Alzheimer’s disease is the most common type of Alzheimer’s disease, representing more than 95% of cases,” said senior author Andrew Yoo, a professor of developmental biology. “It has been very difficult to study in the lab due to the complexity of the disease stemming from various risk factors, including aging as an important contributor. Until now, we did not have a way to capture the effects of aging in the cells to study late-onset Alzheimer’s.”
To date, animal studies of Alzheimer’s disease have, by necessity, focused on mice with rare genetic mutations known to cause inherited, early-onset Alzheimer’s in younger people — a strategy that has shed light on the condition but differs from disease development for the vast majority of patients with the sporadic, late-onset form. To more faithfully recapitulate the disease in the lab, Yoo’s team turned to an approach called cellular reprogramming.
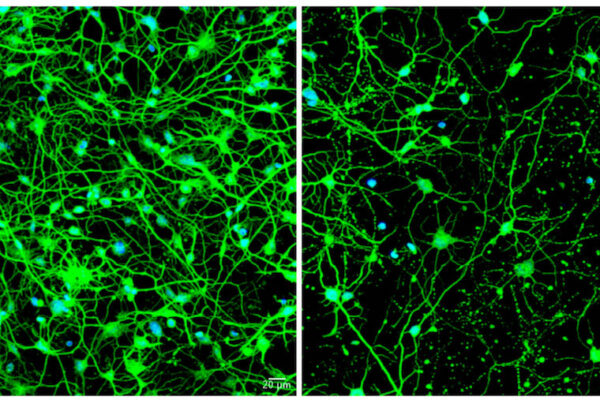
The method to transform easily obtained human skin cells from living patients directly into neurons makes it possible to study Alzheimer’s effects on the brain without the risk of a brain biopsy and in a way that retains the consequences of the patient’s age on the neurons. Past work by Yoo and his colleagues, who pioneered this transformation technique using small RNA molecules called microRNAs, has focused on understanding the development of Huntington’s disease — an inherited neurological condition that typically shows adult-onset symptoms.
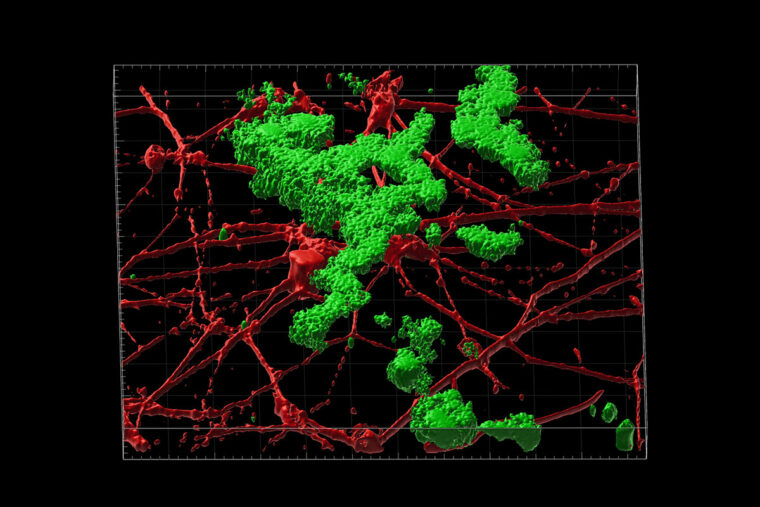
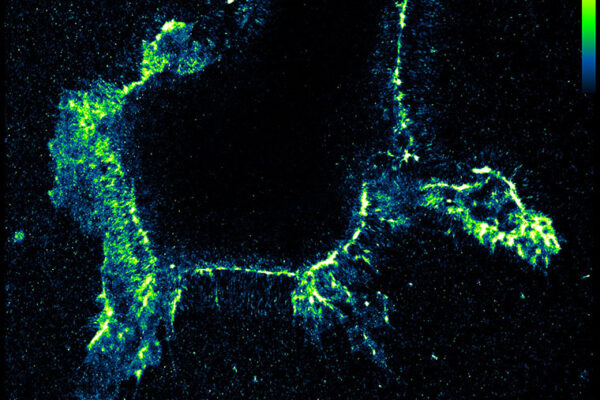
After transforming skin cells into brain cells, the researchers found that the new neurons can grow in a thin gel layer or self-assemble into small clusters — called spheroids — mimicking the 3D environment of the brain. The researchers compared neuronal spheroids generated from patients with sporadic, late-onset Alzheimer’s disease, inherited Alzheimer’s disease and healthy individuals of similar ages.
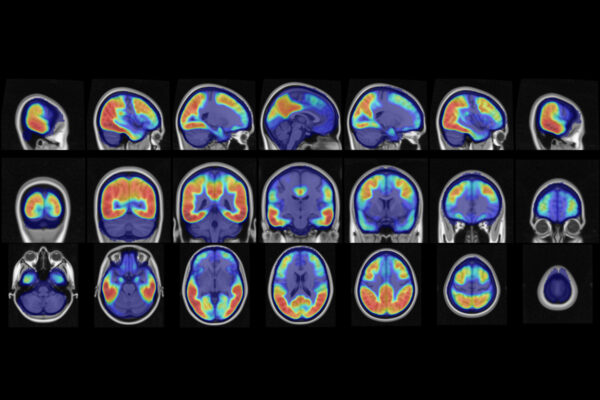
The Alzheimer’s disease patients’ spheroids quickly developed amyloid beta deposits and tau tangles between neurons. Activation of genes associated with inflammation also emerged, and then the neurons began to die, mimicking what is seen in brain scans of patients. Spheroids from older, healthy donors in the study showed some amyloid deposition but much less than those from patients. The small amyloid deposits in older, healthy spheroids are evidence that the technique is capturing the effects of age and suggest that amyloid beta and tau accumulation correlated with aging. It further demonstrates that the Alzheimer’s disease process makes the buildup far worse.
The researchers, including first author Zhao Sun, a staff scientist in Yoo’s lab, found that treating spheroids from late-onset Alzheimer’s disease patients with drugs that interfere with the formation of amyloid beta plaques early in the disease process, before neurons start forming toxic amyloid beta buildup, significantly reduced the amyloid beta deposits. But treating at later time points, after some buildup was already present, had no effect or only modestly reduced subsequent amyloid beta deposits. Such data emphasize the importance of identifying and treating the disease early.
The study further found a role for retrotransposable elements — small pieces of DNA that jump to different locations in the genome — in the development of late-onset Alzheimer’s disease. Inhibition of such “jumping genes” with the drug lamivudine (also called 3TC) — an anti-retroviral drug that can dampen the activity of retrotransposable elements — had a positive effect: The spheroids from late-onset Alzheimer’s disease patients had reduced amyloid beta and tau tangles and showed less neuronal death compared with the same spheroids treated with a placebo. Lamivudine treatment had no beneficial effect on spheroids from patients with early-onset, inherited Alzheimer’s disease, providing evidence that sporadic late-onset Alzheimer’s development related to aging has distinct molecular features compared with inherited autosomal dominant Alzheimer’s disease.
“In these patients, our new model system has identified a role for retrotransposable elements associated with the disease process,” Yoo said. “We were pleased to see that we could reduce the damage with a drug treatment that suppresses these elements. We look forward to using this model system as we work toward new personalized therapeutic interventions for late-onset Alzheimer’s disease.”
The researchers are planning future studies with spheroids that include multiple types of brain cells, including neurons and glia.
Sun Z, Kwon J, Ren Y, Chen S, Walker CK, Lu X, Cates K, Karahan H, Sviben S, Fitzpatrick JA, Valdez C, Houlden H, Karch CM, Bateman RJ, Sato C, Mennerick SJ, Diamond MI, Kim J, Tanzi RE, Holtzman DM, Yoo AS. Modeling late-onset Alzheimer’s disease neuropathology via direct neuronal reprogramming. Science. Aug. 2, 2024. DOI: 10.1126/science.adl2992
An application for a U.S. patent related to this work has been filed by Washington University, titled “Three-dimensional direct neural reprogramming to model Alzheimer’s disease in human neurons,” under application number 020529/US-NP.
This work was supported by the Farrell Family Fund for Alzheimer’s Disease; the Cure Alzheimer’s Fund; the Centene Fund; a Mallinckrodt Scholar Award, a Washington University NeuroGenomics and Informatics Center (NGI) Pilot Award; the Children’s Discovery Institute of Washington University and St. Louis Children’s Hospital, grant numbers CDI-CORE-2015-505 and CDI-CORE- 2019-813; The Foundation for Barnes-Jewish Hospital, grant numbers 3770 and 4642; and the National Institutes of Health (NIH), grant numbers RF1AG056296, R01NS107488, R01AG0789640 and AG066444.
About Washington University School of Medicine
WashU Medicine is a global leader in academic medicine, including biomedical research, patient care and educational programs with 2,900 faculty. Its National Institutes of Health (NIH) research funding portfolio is the second largest among U.S. medical schools and has grown 56% in the last seven years. Together with institutional investment, WashU Medicine commits well over $1 billion annually to basic and clinical research innovation and training. Its faculty practice is consistently within the top five in the country, with more than 1,900 faculty physicians practicing at 130 locations and who are also the medical staffs of Barnes-Jewish and St. Louis Children’s hospitals of BJC HealthCare. WashU Medicine has a storied history in MD/PhD training, recently dedicated $100 million to scholarships and curriculum renewal for its medical students, and is home to top-notch training programs in every medical subspecialty as well as physical therapy, occupational therapy, and audiology and communications sciences.
Originally published on the School of Medicine website