Researchers at Washington University School of Medicine in St. Louis have received a grant from the Centers for Disease Control and Prevention (CDC) totaling $12.5 million to investigate the real-world effectiveness of influenza and COVID-19 vaccines and the immune response to infection and vaccination against these two illnesses.
Unlike a strictly controlled clinical trial, this research is aimed at understanding how vaccination strategies work for people living and working in the community, where they may not receive vaccines and boosters on a strict schedule, or from a single vaccine maker.
“We want to understand how these vaccines work in the real world,” said principal investigator Stacey L. House, MD, PhD, an assistant professor of emergency medicine. “These vaccines have proven to be effective in clinical trials. But we don’t know what it means for the immune response if second doses are delayed, or if boosters are taken at vastly different times, or if people switch vaccine manufacturers for their third or fourth dose, for example. By enrolling large numbers of patients and gathering many data points about them, we hope to understand how effective vaccines are in a diverse community.”
The School of Medicine is one of seven sites enrolling patients in this CDC study. The others are the University of Michigan, Baylor Scott & White Health, Kaiser Permanente Washington, the University of Pittsburgh, University Hospitals Cleveland, and Arizona State University. Duke University will serve as the study’s coordinating center.
As part of the vaccine effectiveness project, House and her team will seek to enroll at least 5,000 participants in the St. Louis region over the grant’s five years. Patients — adults and children — who come to Barnes-Jewish Hospital, Missouri Baptist Medical Center and St. Louis Children’s Hospital with respiratory tract infections will be tested for influenza and COVID-19 and can choose to participate in the study. House said the investigators will collect data on participants’ vaccine history and general medical history and will follow them over time to collect data on any complications patients may experience from these viral infections.
“The abundance of data we will collect on these patients should allow us to see how pre-existing conditions, medications and social determinants of health, such as education and access to health care, may affect vaccine effectiveness and how well patients recover after these infections,” said House, who is also vice chair for clinical research in the Department of Emergency Medicine as well as director of the Emergency Care Research Core.
The researchers also will perform subtype analysis and viral genome sequencing on viral samples from patients to identify and track new viral variants that emerge over time. These samples and sequences will be made available for further research through a national repository that is part of the CDC’s U.S. Flu Vaccine Effectiveness Network.
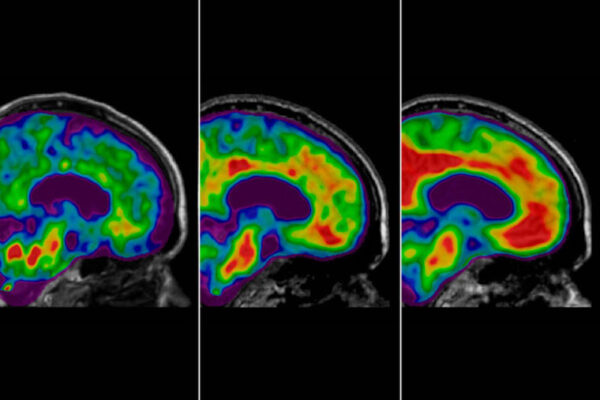
A second project will analyze immune responses to various COVID-19 and influenza vaccines. Led by infectious disease specialists Rachel Presti, MD, PhD, an associate professor of medicine, and Jane O’Halloran, MD, PhD, an associate professor of medicine, researchers will collect samples from patients at specific time points before and after receiving a COVID-19 or influenza vaccine. The samples will be used to assess antibody levels as well as the responses of B cells and T cells, key components of the body’s immune system, to vaccination.
The study aims to answer key questions about vaccination, including how long and robust the immune response from vaccination is; how broad the antibody response is; and how repeated exposure to different viral variants impacts the length and breadth of B cell and T cell responses to viral respiratory infections.
“The CDC has to make vaccine recommendations based on available information, and we don’t have as much data as we would like on the effectiveness of these vaccines outside of clinical trials,” House said. “If we have the kind of detailed data that we hope to gather during this study, the recommendations can start to be a bit more specific for individual patient populations.”
About Washington University School of Medicine
WashU Medicine is a global leader in academic medicine, including biomedical research, patient care and educational programs with 2,700 faculty. Its National Institutes of Health (NIH) research funding portfolio is the fourth largest among U.S. medical schools, has grown 54% in the last five years, and, together with institutional investment, WashU Medicine commits well over $1 billion annually to basic and clinical research innovation and training. Its faculty practice is consistently within the top five in the country, with more than 1,790 faculty physicians practicing at over 60 locations and who are also the medical staffs of Barnes-Jewish and St. Louis Children’s hospitals of BJC HealthCare. WashU Medicine has a storied history in MD/PhD training, recently dedicated $100 million to scholarships and curriculum renewal for its medical students, and is home to top-notch training programs in every medical subspecialty as well as physical therapy, occupational therapy, and audiology and communications sciences.