To help unravel the mysteries of COVID-19, scientists are sequencing the DNA of young, healthy adults and children who develop severe illness despite having no underlying medical problems. The researchers are looking for genetic defects that could put certain individuals at high risk of becoming severely ill from the novel coronavirus.
The McDonnell Genome Institute at Washington University School of Medicine in St. Louis is one of more than 30 genome sequencing hubs worldwide participating in the study. Rheumatologist Megan A. Cooper, MD, PhD, an associate professor of pediatrics, is leading the research at Washington University. Called the COVID Human Genetic Effort, the international project is co-led by the National Institute of Allergy and Infectious Diseases of the National Institutes of Health (NIH), and Rockefeller University.
The researchers also plan to study people who never become infected with SARS-CoV-2, the virus that causes COVID-19, despite repeated exposures. Such individuals may have genetic variations that protect against infection. For example, certain rare genetic variants are known to thwart some types of viral infections, including HIV and norovirus. Knowledge gained from understanding COVID-19’s extremes — unusual susceptibility and resistance — could lead to new therapeutic strategies for the illness.
“The first focus of our study will be patients with severe responses to SARS-CoV-2 infection — severe enough to require intensive care — who appear otherwise healthy and are younger than 50,” said Cooper, who also leads the clinical immunology program and the Jeffrey Modell Diagnostic and Research Center for Primary Immunodeficiencies at St. Louis Children’s Hospital.
“These patients don’t have uncontrolled diabetes, heart disease, chronic lung disease or any other condition that we know increases the risk of severe complications from COVID-19,” she said. “For example, we sometimes see stories about, say, a marathon runner or a generally fit, healthy person who nevertheless got very sick from this virus, or the few healthy children who are getting very sick with COVID-19. These are the kinds of patients we’re interested in for this study. A small proportion of hospitalized patients will fit this category, likely less than 10%.”
Cooper studies primary immunodeficiencies in children. Primary immunodeficiencies are a group of more than 450 genetic disorders of the immune system. They often are caused by mutations in single genes that affect different aspects of immunity.
“With this pandemic, we can use our skills in gene hunting to search for genes that might be associated with severe COVID-19 in children and younger adults,” she said. “We can foresee a future ability to do a genetic sequencing test for individual patients hospitalized with SARS-CoV-2 and get an idea of whether they are likely to need more intensive care. In the meantime, we will be able to learn a great deal about how the immune system responds to this virus and what it needs to be able to respond effectively and in an appropriate manner.”
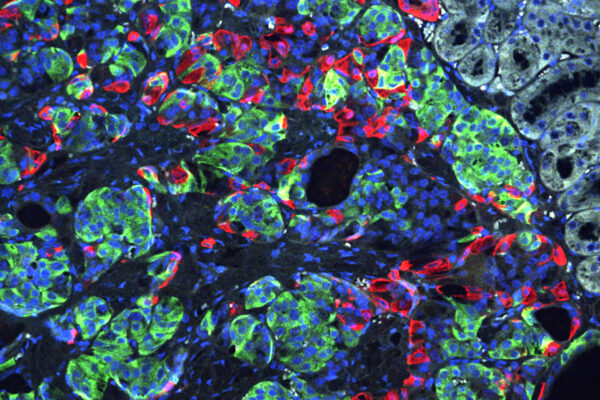
These patients’ genetics could reveal the important immune pathways that the body needs to fight the virus. That knowledge could lead to therapies that also could help other patients who don’t have a genetic susceptibility to the virus but perhaps have high-risk conditions, such as diabetes or heart disease.
“Our immune systems have never seen this virus before,” Cooper said. “We’re seeing severe COVID-19 complications play out across the world right now. It is going to take a global effort to investigate the genetic factors and the immune system factors that really control this infection.”
Research related to COVID-19, including collecting and distributing of patient samples, is managed through Washington University’s Institute of Clinical and Translational Sciences (ICTS), led by William G. Powderly, MD, who is also the Larry J. Shapiro Director of the Institute for Public Health, the J. William Campbell Professor of Medicine and co-director of the Division of Infectious Diseases.