In the face of the COVID-19 pandemic, a diverse team of makers from across Washington University in St. Louis’ Danforth and Medical campuses, Barnes-Jewish Hospital and BJC HealthCare have come together to protect front-line health-care workers and employees on the ground.
“With the surge of COVID-19 patients we’re expecting, we want to make sure doctors, nurses and other health-care providers do not run out of the PPE (personal protective equipment) and other supplies and equipment they need to do their jobs safely and take care of these patients well,” said Thomas M. Maddox, MD, professor of medicine and executive director of the BJC/WUSM Healthcare Innovation Lab.
The COVID-19 WashU/BJC Maker Task Force executive team consists of: Maddox; Ali Kosydor, the lab’s director of operations; Aaron Bobick, dean of the McKelvey School of Engineering; Eric Leuthardt, MD, professor of neurological surgery and inventor; and Philip Bayly, chair of mechanical engineering and materials science. Their varied expertise mirrors that of the larger task force that soon coalesced.
“Working closely with the BJC supply chain organization, we have developed interesting prototypes of PPE and emergency ventilators, received clinical feedback, and worked with local makers and suppliers as necessary to augment the traditional channels,” Bobick said.
“So many doctors and engineers and members of the maker community in St. Louis wanted to apply their skills to help. So, we have brought all of these efforts together to better coordinate the response,” Maddox said.
Developing new products
The Maker Task Force serves as a central hub for St. Louis-area maker efforts to help health-care workers care for patients during the COVID-19 pandemic. The group is working to develop 14 product lines, including isolation gowns, surgical masks, face shields, emergency ventilators, ventilator replacement parts, N95 respirators and methods to disinfect them. Once the products have been developed and tested by the Maker Task Force, they will also need to be vetted and approved by BJC HealthCare before they can be used in the field.
“The task force is doing incredibly important work and in record time,” said Tom Harvieux, chief supply chain officer at BJC HealthCare. “It serves as a vital resource in creating local production capacity of supplies as we care for COVID-19 patients across the region.”
Members of the task force are working with local manufacturers. The goal is to scale up the production of these supplies, which will serve as a backup, supplementing the regular supply chain if vital protective equipment runs out.
Mary Ruppert-Stroescu, associate professor and coordinator of fashion design at the Sam Fox School of Design and Visual Arts, is leading a task force section focused on masks and another focused on gowns. For the latter, she has worked with the BJC supply chain and local manufacturers to design, test and begin large-scale manufacturing of isolation gowns — up to 10,000 pieces per day.

“I’ve been researching innovative ways to engage clothing for health and well-being by collaborating with healthcare and engineering professionals and students for about eight years,” Ruppert-Stroescu said. “The pace and stakes of the current task force is like nothing I have ever experienced.”
In fact, “pace” stands out as one of the most impressive and integral features of the task force.
“It took about a week between coming up with the idea and building something that was working,” Bayly said.
He was referring to building a ventilator, capable of delivering air to patients when they can no longer breathe on their own efficiently.
“We wanted to have something we can put on the shelf,” he said. “Something that, if people said, ‘We need some of these,’ then hundreds could be available in a week.”
‘What clinicians need’
Bayly, the Lilyan & E. Lisle Hughes Professor of Mechanical Engineering, solicited the help of: Jerry Halley, a former student and chief engineer at a company that makes parts for fighter jets; Dennis Mell, an electrical engineer and professor of practice at the university; and machinist John Kreitler, of the Instrument Machine Shop at the School of Medicine.
After that initial week, Bayly said, they solicited feedback from Broc Burke, MD, PhD, instructor in anesthesiology, and others at the School of Medicine, and, about a week later, their ventilator was undergoing tests in a clinical simulation lab. “It’s not anywhere near a human patient,” he said — it’s on a dummy that mimics patient behavior.
“We’re not medical people,” Bayly said. “We’re making something clinicians can evaluate.”
Leuthardt agreed: “We need to be able to understand what clinicians need and take it to the engineers and the makers and come up with solutions. One element that we’re working on is a mobile app that allows health-care workers on the front lines to identify what they need. We want to be able to monitor that in real time and quickly respond so, ideally, they never run out of key supplies.”
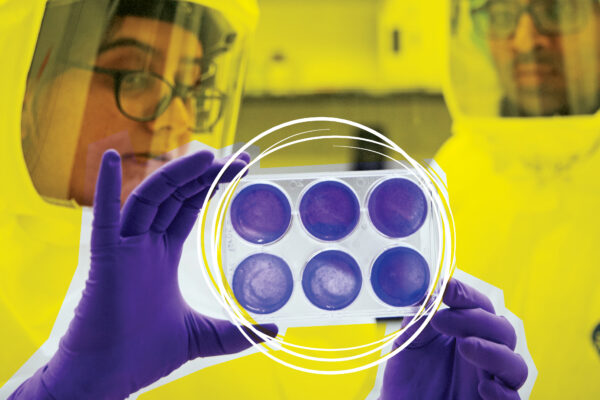
Anticipating a possible shortage of N95 respirator masks, for example, led Jennifer K. Lodge, vice chancellor for research, to reach out to Nirah Shomer, DVM, PhD, associate vice chancellor for veterinary affairs and director of the Division of Comparative Medicine, and Susan Cook, director of the Office of Biological Safety, because of their teams’ experience using vaporized hydrogen peroxide to sterilize lab spaces.
Studies have shown that the technique could be adapted to disinfect large numbers of N95 respirators, a special type of mask that is particularly effective at filtering out fine aerosols. The virus that causes COVID-19 is mostly spread through larger droplets that can be blocked by simpler masks. But many procedures that health-care providers perform, such as intubation to help a patient breathe, produce virus-spreading aerosols, requiring that higher level of protection.
Harnessing existing equipment, the task force is building the capacity to disinfect up to 6,000 N95 respirators per day. According to Andrew Pierce, director of supply and perioperative business at Barnes-Jewish Hospital, each health-care worker places his or her own N95 into a gas-permeable bag and writes his or her department and name on the bag so the respirators can be disinfected and returned.
“Returning the specific respirator to its original wearer is an important element of our process,” Pierce said. “No one else touches the N95s after they’ve been bagged and sealed. That provides a lot of confidence that we’re handling these respirators well and returning them in a safe and clean way.”
The group also is anticipating the possibility of needing respirators manufactured from alternative materials that reproduce the characteristics of an N95 in a reliable way.
Low-tech solutions
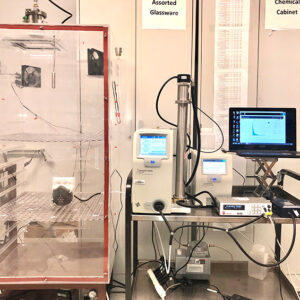
At the McKelvey School of Engineering’s Center for Aerosol Science & Engineering (CASE), two labs are currently testing materials for and designing prototypes of such respirators. The testing is being guided by Brent Williams, the Raymond R. Tucker Distinguished InCEES Career Development Associate Professor; and Pratim Biswas, assistant vice chancellor, chair of energy, environmental and chemical engineering, the Lucy & Stanley Lopata Professor and head of the Aerosol and Air Quality Research Laboratory.
“We have a collaborative team of CASE researchers characterizing filtration materials and testing the stability and performance of N95-type respirators after they have undergone disinfection treatment for reuse,” Williams said. In addition, the aerosol team is investigating “low-tech” solutions with common household materials that the public can use.
“We want to create a library of materials that we have already tested that we know will work, no matter what resources may be available at the time,” said task force member Kate Meacham, MD, PhD, assistant professor of anesthesiology. “We don’t want to find ourselves in a situation where we develop a great solution to a respirator problem, for example, but then the materials dry up.”
This library is already taking shape; design specifications for “The WashU Shield,” developed in the Spartan Light Metal Products Makerspace, are available on the task force website.
Wyly Brown, assistant professor of architecture, along with Sam Fox School facilities manager Leland Orvis and instructional technician Matthew Branham, is helping coordinate production printing and parts-cutting for those shields, which were designed by McKelvey Engineering‘s Ruth Okamoto, teaching professor of mechanical engineering and materials science and Maker Space director, and Charlotte Guertler, staff research associate and Maker Space associate director.
Brown and Orvis also are working with Ruppert-Stroescu to develop molded masks in the style of the N95.

“It is inspiring to see McKelvey Engineering faculty, students and staff working with colleagues across the university and beyond, all rising to the occasion to help ensure our medical colleagues both at BJC/WUSM and in the region have access to the equipment and supplies they require,” Bobick said.
The unprecedented nature of these collaborations, across departments, campuses and outside industries has ultimately been driven by a singular, urgent goal.
“The safety of the front-line health-care workers is on the line,” Meacham said. “Everyone understands the stakes. With this incredible team, you can pick up the phone and make something important happen in 24 hours. With everyone focused on the same goal, this group has been able to move mountains.”
— Brandie Jefferson, senior news director, Liam Otten, senior news director, and Julia Evangelou Strait, senior medical science writer, all contributed to this report.
WashU Response to COVID-19
Visit coronavirus.wustl.edu for the latest information about WashU updates and policies. See all stories related to COVID-19.