When a public building catches fire, its built-in systems automatically respond: Smoke alarms blare, sprinklers turn on and occupants quickly evacuate.
What if the life-threatening danger isn’t fire, but invisible airborne contaminants that can make occupants sick? Could a similar smart-building system monitor and improve air quality indoors, where Americans spend 90% of their time?
The Advanced Research Projects Agency for Health (ARPA-H) has awarded a contract of up to $40 million to a multi-institutional research team led by Virginia Tech. Washington University in St. Louis is leading one of three technical areas and will receive $15 million to develop commercial-ready devices that disrupt the transmission of infectious disease.
The WashU project is led by Rajan Chakrabarty, a professor of energy, environmental and chemical engineering. Researchers at the University of Michigan, Yale and Emory universities also will receive subawards from WashU.
“McKelvey Engineering and WashU are delighted to be a part of this nationwide ambitious research, which has the potential to change how we deal with airborne pathogens and have a positive impact on human health,” said Aaron F. Bobick, dean and the James M. McKelvey Professor in the McKelvey School of Engineering at WashU. “Rajan Chakrabarty and his collaborators have already made fundamental contributions in this domain, and we are excited to see how this technology evolves.”
The research project, called Bioaerosol Risk Assessment interVention Engineering (BRAVE), aims to reduce respiratory illnesses such as cold, flu and asthma by 25% with an innovative clean-air version of a fire suppression system. Ultimately, the team plans to commercialize its research so that the whole-building system — including biosensors, software and engineering interventions — becomes a turnkey technology widely available for installation in buildings.
“Developing a cost-efficient technology that is capable of detecting tens of viruses, fungi, allergens and bacteria in indoor air in real time is nothing short of a moonshot,” said Chakrabarty, WashU’s team lead. “It’s a grand challenge, but it’s exciting in the sense that here is an opportunity to really push the envelope of what is possible. If successful, this technology can create a prevention mechanism to avert future pandemics.”

Here’s how the technology works:
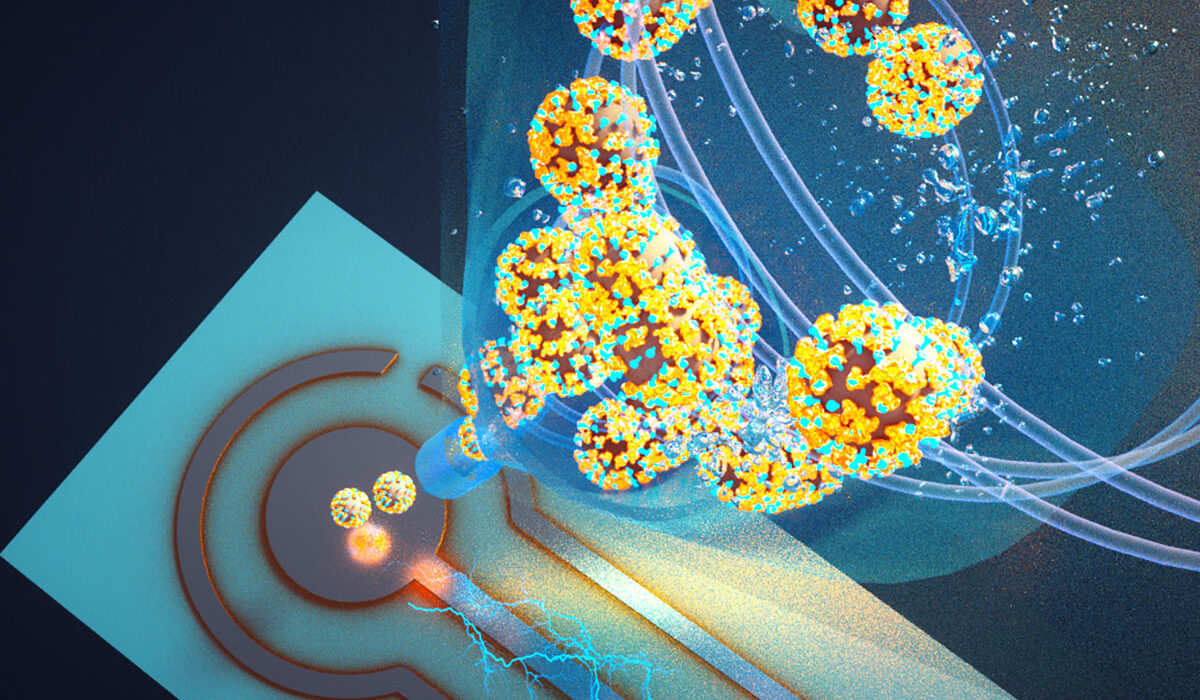
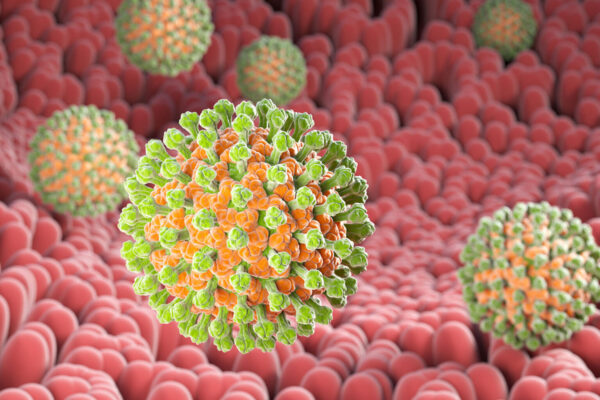
· A biosensor acts like a smoke alarm, detecting in real time 25 viruses, bacteria, allergens and fungi in the air, including SARS-CoV-2, influenza, respiratory syncytial virus, Legionella and Stachybotrys chartarum, commonly known as black mold.
·Next, a suite of computational modeling software analyzes data from the building’s biosensors and other sources to assess risk for occupants.
· When the risk is high, the sensor automatically communicates with the building’s HVAC system to amp up building ventilation with more outdoor air, to increase filtration or to turn on germicidal UV lights in the ducts — interventions that have been proven to reduce concentrations of bioaerosols and reduce risk of illness.
· The system may even issue alerts and recommend behavior changes, such as going outside or reducing building occupancy. But most of the time, it will operate in the background, adjusting conditions as quietly as a thermostat.
The multi-institutional project is led by Linsey Marr, a professor at Virginia Tech, along with Aaron J. Prussin II, senior project manager.
“The knowledge that comes out of this project will mean that when you go into a classroom, office, restaurant or other building that has adopted the solutions from this research, the air is going to be cleaner and safer than it was before,” said Marr, who was recognized in 2023 with a MacArthur “genius grant” for her research into air quality and the transmission of infectious bioaerosols. “That will mean that you have fewer days of illness, fewer missed workdays and a better quality of life.”
The team will conduct the initial round of testing in day care centers, where “there are a lot of pathogens around, kids are getting sick, and their illness impacts parents and the whole community,” Marr said. “It’s like a fire, and you want to put out the fire where it starts.”
What researchers learn there will be relevant in almost any communal setting, including classrooms, supermarkets, hospitals and airports. With the BRAVE approach implemented in these buildings, researchers expect fewer children, parents and workers will get sick, leading not only to higher levels of health and well-being, but to reduced absenteeism and improved productivity, making clear that better indoor air quality is worth the investment.
Additional WashU collaborators include:
- Michael Vahey, associate professor of biomedical engineering, McKelvey Engineering
- Meng Xu, senior staff scientist, energy, environmental and chemical engineering, McKelvey Engineering
- Carolina Lopez, Theodore and Bertha Bryan Professorship in Environmental Medicine, professor of molecular microbiology, WashU Medicine
- John Cirrito, professor of neurology, WashU Medicine
- Carla Yuede, professor of psychiatry, of neuroscience and of neurology, WashU Medicine
ARPA-H is a government agency within the U.S. Department of Health and Human Services that supports the development of high-impact solutions to society’s most challenging health problems. Its Building Resilient Environments for Air and Total Health program, through which the team’s grant is funded, focuses on smart-building systems that monitor and respond to changes in indoor air quality as a way to revolutionize public health.
The initial round of funding is $20 million, with additional tranches up to $40 million over the next five years.
Melody Warnick of Virginia Tech contributed to this news release.