COVID-19 vaccination elicited antibody responses in nearly nine out of 10 people with weakened immune systems, although their responses were only about one-third as strong as those mounted by healthy people, according to a study by researchers at Washington University School of Medicine in St. Louis.
The study, published Aug. 30 in the Annals of Internal Medicine, looked at people taking immunosuppressive medications to treat chronic inflammatory diseases such as inflammatory bowel disease and rheumatoid arthritis. Since a minimum level of antibodies needed for protection hasn’t been established, it has been difficult to say whether the levels achieved by people on immune suppressing drugs are high enough to protect them from severe COVID-19, the researchers said. The Centers for Disease Control and Prevention (CDC) recently recommended that people taking immunosuppressants receive a third dose of the vaccine to strengthen their immune responses.
Nonetheless, the discovery that COVID-19 vaccination elicits a response in people with compromised immune systems — even if not quite as strong a response — is encouraging news for a population that faces a high risk of serious illness.
“Some of our patients have been hesitant about getting vaccinated, which is unfortunate because they are at increased risk of having more severe cases of COVID-19 if they happen to get infected, compared to those not taking immune suppressing drugs,” said co-senior author Alfred Kim, MD, PhD, an assistant professor of medicine who treats patients with autoimmune conditions at Barnes-Jewish Hospital. “Some of them are worried that vaccination might cause their disease to flare, but we haven’t seen that happen. Others don’t see the point of vaccination, because they think the drugs they’re taking to treat their autoimmune condition will prevent them from producing an immune response to the vaccine. What we found here is that the vast majority of immunocompromised patients with autoimmune diseases are able to mount antibody responses following COVID-19 vaccination. There’s clearly a benefit for this population.”
When the first COVID-19 vaccines were authorized for emergency use in December 2020, Kim worried about how well they would work for his patients. Previous studies had shown that immunosuppressive medications can blunt people’s responses to other vaccines, such as those for influenza and pneumococcal diseases.
Kim and co-senior author Ali Ellebedy, PhD, associate professor of pathology and immunology, of medicine and of molecular microbiology, set out to determine how well people taking immunosuppressive drugs respond to COVID-19 vaccination. Co-first authors Parakkal Deepak, MBBS, assistant professor of medicine in the Division of Gastroenterology, Wooseob Kim, PhD, a postdoctoral researcher in Ellebedy’s lab, and Michael Paley, MD, PhD, an instructor in medicine in the Division of Rheumatology, with the help of other colleagues at Washington University and the University of California, San Francisco, pulled together a participant group comprising 133 patients and 53 healthy people for comparison. The patients each were taking at least one immune-suppressing medication for illnesses such as inflammatory bowel disease, rheumatoid arthritis, spondyloarthritis, lupus and multiple sclerosis.
Participants provided blood samples within two weeks before receiving the first dose of the Pfizer or Moderna vaccine and within three weeks after receiving the second dose. The researchers measured each participants’ antibody levels and counted the number of antibody-producing cells in their blood samples. All patients stayed on their prescribed drug regimens, except for three whose medications were paused within one week of immunization.
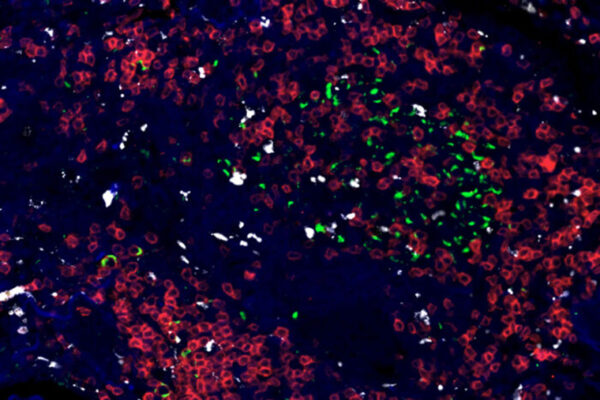
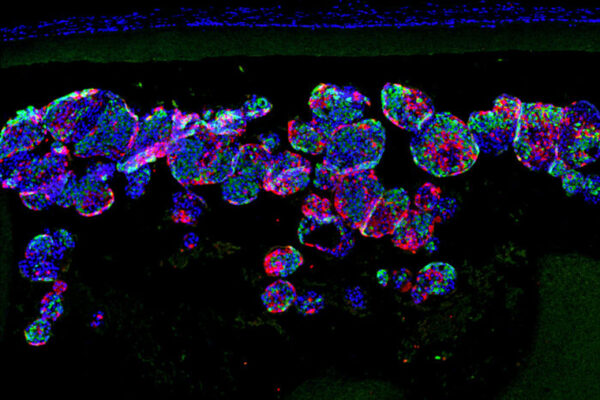
All healthy participants and 88.7% of the immunosuppressed participants produced antibodies against the virus that causes COVID-19. However, antibody levels and the number of antibody-producing cells in the immunosuppressed group were one-third as high as those in the healthy group.
“Nobody knows what minimum level of antibodies is needed for protection,” Ellebedy said. “We just don’t know whether people who had low but detectable levels of antibodies are protected or not. It’s that uncertainty that justifies the need for a third dose, especially since we have these highly infectious variants that are capable of causing breakthrough infections even among healthy people.”
Two classes of drugs led to particularly weak immune responses. Only 65% of people taking glucocorticoids and 60% of people taking B cell-depleting therapies developed detectable antibody responses. People taking antimetabolites such as methotrexate, TNF inhibitors or JAK inhibitors, on the other hand, did not generate significantly weaker immune responses than people not taking those drugs.
Alfred Kim, Ellebedy and colleagues are preparing to follow the same group of participants as they receive their third shots. If a third dose allows people on immunosuppressants to achieve the antibody levels seen in healthy people after a second dose, Alfred Kim said he would feel better about how well the vaccine protects his patients.
“Receiving this additional dose may help mitigate this loss of response,” he said. “It’s really important for people who are immunocompromised to receive this dose to maximize their ability to protect themselves from SARS-CoV-2.”
Deepak P, Kim W, Paley MA, Yang M, Carvidi AB, Demissie EG, El-Qunni AA, Haile A, Huang K, Kinnett B, Liebeskind MJ, Liu Z, McMorrow LE, Paez D, Pawar N, Perantie DC, Schriefer RE, Sides SE, Thapa M, Gergely M, Abushamma S, Akuse S, Klebert M, Mitchell L, Nix D, Graf J, Taylor KE, Chahin S, Ciorba MA, Katz P, Matloubian M, O’Halloran JA, Presti RM, Wu GF, Whelan SPJ, Buchser WJ, Gensler LS, Nakamura MS, Ellebedy AH, Kim AHJ. Effect of Immunosuppression on the Immunogenicity of mRNA Vaccines to SARS-CoV-2: A Prospective Cohort Study. Annals of Internal Medicine. Aug. 30, 2021. DOI: 10.7326/M21-1757
This research was supported by The Leona M. and Harry B. Helmsley Charitable Trust; the Marcus Program in Precision Medicine Innovation; the National Center for Advancing Translational Sciences of the National Institutes of Health (NIH), grant number UL1 TR002345; and National Institute of Arthritis and Musculoskeletal and Skin Diseases of the NIH, grant number P30AR070155.
Washington University School of Medicine’s 1,700 faculty physicians also are the medical staff of Barnes-Jewish and St. Louis Children’s hospitals. The School of Medicine is a leader in medical research, teaching and patient care, consistently ranking among the top medical schools in the nation by U.S. News & World Report. Through its affiliations with Barnes-Jewish and St. Louis Children’s hospitals, the School of Medicine is linked to BJC HealthCare.