A new AI-based technology that rapidly maps the brain to locate sensitive areas that control speech, vision, movement and other critical functions has received authorization from the Food and Drug Administration (FDA), enabling it to be marketed to hospitals with the aim of enhancing the precision of neurosurgeries. The technology was developed by researchers and clinicians at Washington University School of Medicine in St. Louis to more precisely guide neurosurgeons in performing delicate brain surgeries to remove tumors or treat epilepsy, for example.
The Cirrus Resting State fMRI Software is being brought to market by Sora Neuroscience Inc., a WashU startup company that licensed the technology from the university. The technology is built on decades of WashU Medicine leadership in the field of neuroscience and functional imaging of the brain. Its development has been funded by the National Institutes of Health (NIH), with the support of private investors.
“This is going to be a sea change for clinical imaging and brain mapping,” said Eric C. Leuthardt, MD, the Shi H. Huang Professor of Neurological Surgery, who developed the technology at WashU Medicine and co-founded Sora Neuroscience. “Now clinicians have access to a broader and more accessible way to look at brain function that can quickly provide insights across neurosurgery applications and for brain diseases, which will benefit patients.”
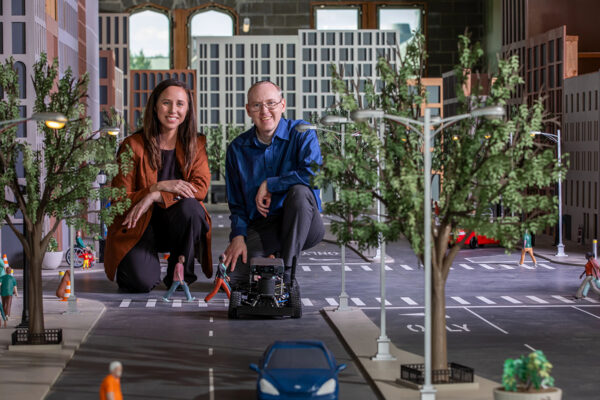
The development of Cirrus software highlights the vital role academic entrepreneurs and startup companies play in translating discoveries into real-world solutions that improve people’s lives, said Doug E. Frantz, PhD, vice chancellor for innovation and commercialization at WashU.
“Transforming years of scientific advances into a tool that surgeons can use in the operating room is only possible through partnerships with commercial ventures like Sora Neuroscience and the WashU Medicine faculty who helped launch the company,” Frantz said. “This is a clear example of how entrepreneurship drives the translation of groundbreaking research from the lab to patient care.”
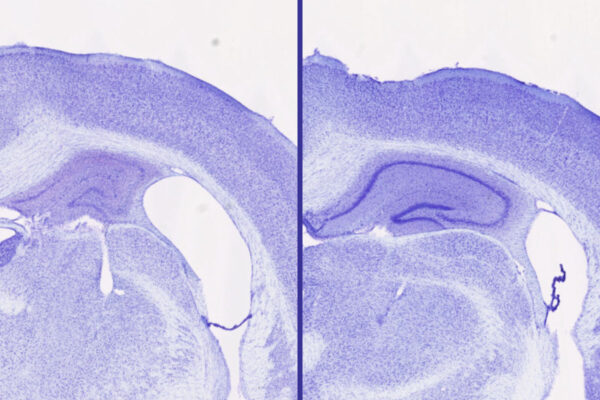
The Cirrus Resting State fMRI software can identify distinct networks of brain activity that govern key activities such as language, vision and movement, and create maps of their locations. Typically, such maps require specialized staff and up to an hour in a scanner to map such networks. The algorithms in the Cirrus software, which are based on artificial intelligence technology, can analyze patterns of linked activity in a resting brain that are known to correspond to specific brain functions. They can complete their mapping of multiple brain networks from as few as 12 minutes of functional magnetic resonance imaging (fMRI), which tracks changes in the brain’s blood flow to identify areas of neurological activity.
The scans for the Cirrus software are performed while a person is at rest in the MRI machine, as opposed to performing a task such as speaking or moving fingers and toes to activate specific brain networks. Leuthardt explained that task-based fMRI is only able to create usable maps for surgeons approximately two-thirds of the time, typically due to patient movement or inability to participate in the task. In contrast, 87% of Cirrus’ scans can be reliably incorporated into a surgeon’s operating plan.
Task-based fMRI is also limited to those who can perform these tasks and follow instructions. For that reason, Cirrus Resting State fMRI software procedure will make fMRI mapping available to a much larger group of patients, said Joshua Shimony, MD, PhD, a professor of radiology at WashU Medicine Mallinckrodt Institute of Radiology, who was a co-investigator with Leuthardt on the studies underlying the technology and is also a scientific adviser to Sora Neuroscience.
“Resting state fMRI can be done on patients who have difficulty with task-based fMRIs, such as children, patients who are confused or who need sedation or anesthesia, or those who are hard of hearing or don’t speak English,” he said.
Leuthardt said that while the technology was initially developed in his laboratory, the underlying data drew from decades of WashU Medicine-led research on resting-state fMRI imaging. Carl Hacker, MD, PhD, who recently completed his WashU neurosurgery residency training, developed the AI-based algorithms driving the Cirrus program while he was a doctoral student in Leuthardt’s laboratory. Physicians and scientists have collaborated for years to develop and advance the imaging analytic capability for pre-surgical brain mapping and conduct studies on its effectiveness.
WashU’s Office of Technology Management filed the initial patents more than a decade ago and licensed the technology in 2021 to Sora Neuroscience. The company was founded in 2020 by Leuthardt along with Hacker and WashU Medicine professor of radiology Daniel Marcus, PhD, and assistant professor of radiology Mikhail Milchenko, PhD.
About Washington University School of Medicine
WashU Medicine is a global leader in academic medicine, including biomedical research, patient care and educational programs with 2,900 faculty. Its National Institutes of Health (NIH) research funding portfolio is the second largest among U.S. medical schools and has grown 83% since 2016. Together with institutional investment, WashU Medicine commits well over $1 billion annually to basic and clinical research innovation and training. Its faculty practice is consistently within the top five in the country, with more than 1,900 faculty physicians practicing at 130 locations and who are also the medical staffs of Barnes-Jewish and St. Louis Children’s hospitals of BJC HealthCare. WashU Medicine has a storied history in MD/PhD training, recently dedicated $100 million to scholarships and curriculum renewal for its medical students, and is home to top-notch training programs in every medical subspecialty as well as physical therapy, occupational therapy, and audiology and communications sciences.
Originally published on the WashU Medicine website