Millions of children in under-resourced parts of the world suffer from malnutrition and, consequently, stunted growth. Protein-based therapeutic foods designed to restore health are lifesavers for many, but a significant number of malnourished children do not respond to available therapies.
But now, researchers at Washington University School of Medicine in St. Louis have found that mice with poor gut health similar to that of malnourished, stunted kids benefited from a therapeutic regime that combines dietary protein with a metabolism-boosting therapy and a bile acid-reducing drug. The findings, published Jan. 3 in Science Translational Medicine, could offer a new approach to treating stunted kids who don’t respond to dietary intervention alone.
“It’s a challenge to help children who don’t respond to therapeutic food,” said Ta-Chiang Liu, MD, PhD, an associate professor of pathology and immunology and the study’s senior author. “Meanwhile, the long-term health consequences on their physical and cognitive development are significant. We are excited about our new findings because we have identified two potentially targetable pathways that may be responsible for the abnormalities in the tissue of the small intestine that we see in these kids. Further, our research indicates that a currently available drug that reduces bile acid potentially could allow these children to respond to food therapy.”
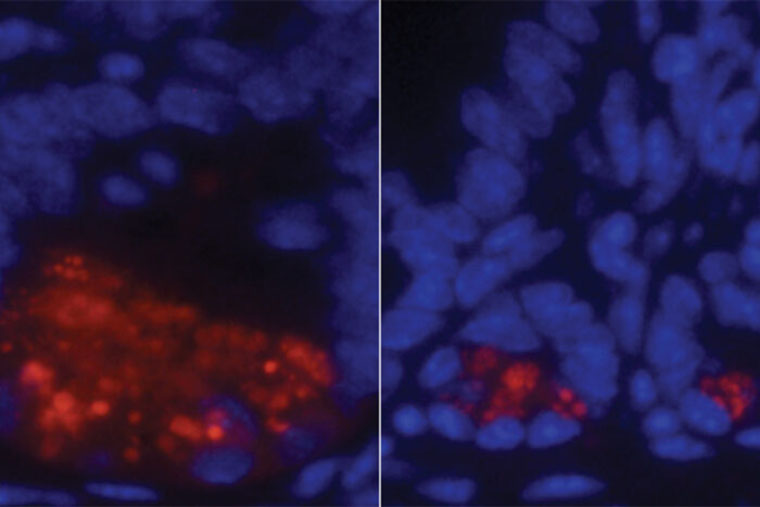
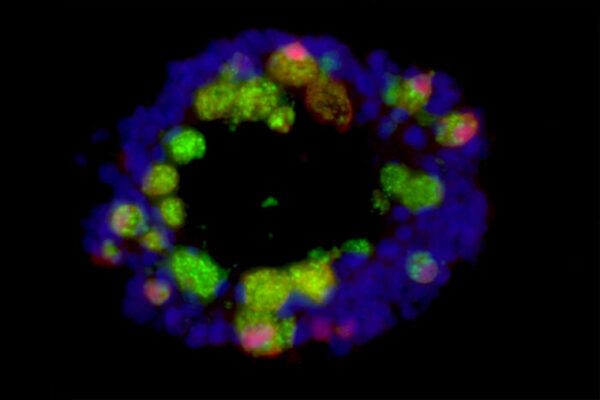
Poor gut health in malnourished children can manifest as a disease — called environmental enteric dysfunction — in the lining of the small intestine. The condition affects nutrient absorption from food and responses to oral vaccines. Nutrient-absorbing, finger-like projections in the small intestine become shortened, and a diminished population of cells responsible for safeguarding against microbes increases infection risk.
The researchers flagged two genetic pathways in the small intestines of 115 Zambian and 52 Pakistani children affected by environmental enteropathy. Forty-two North American children who did not have the disease served as controls and were included in the analysis. The researchers also studied mice with the same gut abnormalities as the affected children. The damaged pathways in both sets of children and mice suggested that a dietary protein deficiency and excess bile acid in the small intestine were harmful to the gastrointestinal tract.
Molecules essential for normal bodily function are derived from diet. Dietary protein is critical for creating and maintaining a supply of a helper molecule — nicotinamide adenine dinucleotide (NAD) — found in all cells and essential for generating energy from food, repairing damaged genetic material and overseeing vital cellular function. When little protein is consumed, the NAD reservoir shrinks, affecting the health of small intestinal cells, the researchers believe.
The researchers found that many of the children in the study with environmental enteric dysfunction were genetically prone to having difficulties converting dietary protein to NAD. Therefore, they determined that drugs that boost NAD levels were necessary. However, feeding sick mice the NAD-boosting drug only partially restored gut health and didn’t completely fix the problem. Adding a bile acid-reducing drug — cholestyramine — along with the NAD-boosting agent restored the health of the small intestinal lining.
Excess bile acids in the small intestine can lead to diarrhea and impair nutrient absorption. Children with this small-intestine condition have increased bile acid levels in their feces, Liu explained. Abnormally high levels of bile acid in the feces of the sick mice mimicked such levels in bile acids of children with like conditions.
“Cholestyramine is an FDA-approved drug already used for reducing bile acid levels in the gut,” explained Liu, who would like to evaluate similar drugs in clinical trials as a potential treatment for malnutrition. “If it works in people when paired with a protein-rich diet to improve the gut defects seen in these kids, we could potentially help children throughout the world.”
Malique A, Sun S, Chandwe K, Amadi B, Haritunians T, Jain U, Muegge BD, Frein J, Sasaki Y, Foster A, Storer CE, Mengesha E, Kern J, McGovern DPB, Head RD, Kelly P, Liu TC. NAD+ precursors and bile acid sequestration treat preclinical refractory environmental enteric dysfunction. Science Translational Medicine. Jan. 3, 2024. DOI: 10.1126/scitranslmed.abq4145
The study was supported by the National Institute of Diabetes and Digestive and Kidney Diseases of the National Institutes of Health (NIH), grant numbers R01 DK125296, R01 DK124274, R01 DK136829 and U01 DK062413; the Bill & Melinda Gates Foundation, grant numbers OPP1066118 and OPP1152812; and the Department of Veterans Affairs, Veterans Health Administration, grant number 1IK2BX004909. This content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Diabetes and Digestive and Kidney Diseases or the NIH.
About Washington University School of Medicine
WashU Medicine is a global leader in academic medicine, including biomedical research, patient care and educational programs with 2,800 faculty. Its National Institutes of Health (NIH) research funding portfolio is the third largest among U.S. medical schools, has grown 52% in the last six years, and, together with institutional investment, WashU Medicine commits well over $1 billion annually to basic and clinical research innovation and training. Its faculty practice is consistently within the top five in the country, with more than 1,800 faculty physicians practicing at 65 locations and who are also the medical staffs of Barnes-Jewish and St. Louis Children’s hospitals of BJC HealthCare. WashU Medicine has a storied history in MD/PhD training, recently dedicated $100 million to scholarships and curriculum renewal for its medical students, and is home to top-notch training programs in every medical subspecialty as well as physical therapy, occupational therapy, and audiology and communications sciences.
Originally published on the School of Medicine website