Washington University pediatric specialists who treat patients at St. Louis Children’s Hospital are part of a major research effort led by the National Institutes of Health (NIH) to investigate how SARS-CoV-2, the virus that causes COVID-19, affects children and young adults up to age 21. This age group accounts for roughly 13% of infections in the United States.
Most children who test positive for the novel coronavirus do not get very sick; many show no symptoms at all. But weeks after infection, a small percentage can develop a condition called multisystem inflammatory syndrome in children (MIS-C), a life-threatening condition marked by severe inflammation of one or more parts of the body, including the heart, lungs, kidneys, brain, skin, eyes and gastrointestinal organs. The syndrome disproportionately affects Black and Hispanic children. Although most children with MIS-C survive, its cause and long-term effects remain largely unknown.
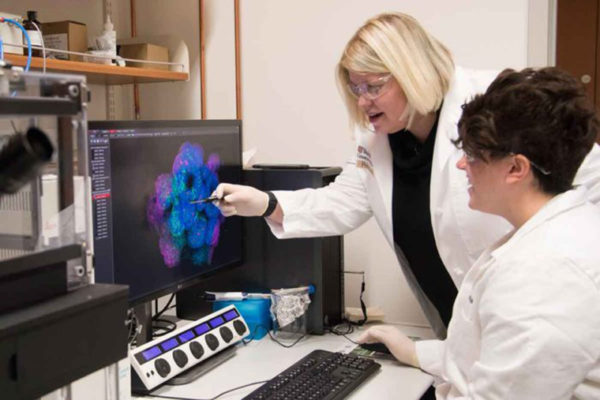
The Washington University researchers are part of the Pediatric Research Immune Network on SARS-CoV-2 and MIS-C (PRISM) clinical trial at St. Louis Children’s Hospital, one of 20 sites nationwide in the study funded by the National Institutes of Allergy and Infectious Diseases. The trial is aimed at understanding the extent to which children and young adults develop serious complications of COVID-19, including MIS-C, that can lead to hospital admission or death. They also will decipher the underlying immunology that leads to different forms of MIS-C and COVID-19 in children. Charles Canter, MD, professor of pediatrics and the Lois B. Tuttle and Jeanne B. Hauck Chair in Pediatric Cardiology, will lead the trial, supported by co-investigators William Orr, MD, and Carol Kao, MD, both assistant professors of pediatrics.
“While MIS-C is rare, it is worrisome because most children hospitalized with the condition were healthy just a few weeks before,” Canter said. “We can’t predict which children will develop it and why. The aim of this study is to understand what drives the development of MIS-C and severe COVID-19 in children so we can identify those who are at risk and determine the best way to treat them.”
Washington University School of Medicine’s 1,500 faculty physicians also are the medical staff of Barnes-Jewish and St. Louis Children’s hospitals. The School of Medicine is a leader in medical research, teaching and patient care, ranking among the top 10 medical schools in the nation by U.S. News & World Report. Through its affiliations with Barnes-Jewish and St. Louis Children’s hospitals, the School of Medicine is linked to BJC HealthCare.