Probiotics – which are living bacteria taken to promote digestive health – evolve once inside the body and have the potential to become less effective and sometimes even harmful, according to a new study from Washington University School of Medicine in St. Louis. The findings suggest that developers of probiotic-based therapeutics must consider how the probiotics might change after administration. (Video: Mark Hallett, Huy Mach and Gaia Remerowski/Washington University School of Medicine)
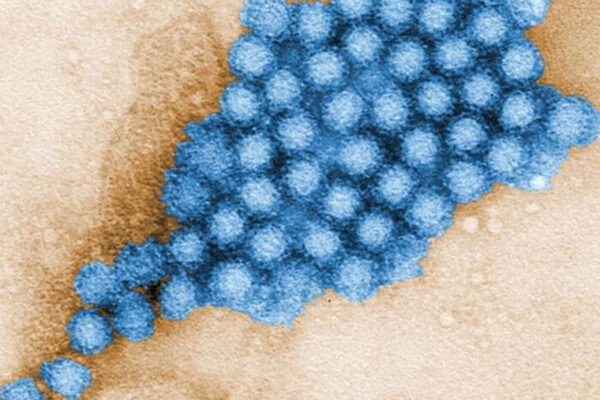
Probiotics – which are living bacteria taken to promote digestive health – can evolve once inside the body and have the potential to become less effective and sometimes even harmful, according to a new study from Washington University School of Medicine in St. Louis.
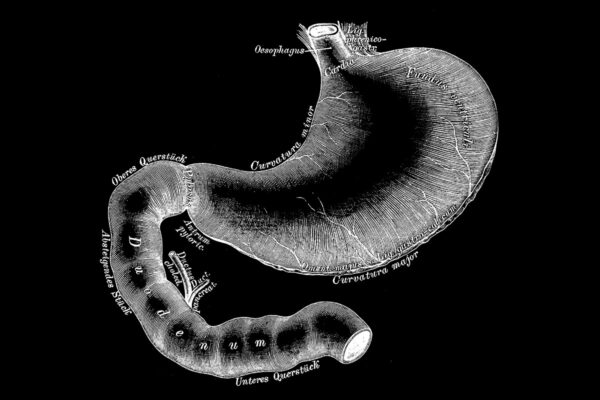
Researchers studying a strain of Escherichia coli (E. coli) bacteria sold in Europe as an anti-diarrheal probiotic found that the bacteria’s DNA changed and they developed new capabilities after living in mice’s intestines for a few weeks. Under some conditions, the probiotics even turned on their hosts and acquired the ability to eat the protective coating on the intestine. Destruction of this layer has been linked to irritable bowel syndrome. The mice’s diets and the make-up of their gut bacterial community influenced how much the probiotic evolved and in what ways.
The findings, published March 26 in Cell Host and Microbe, suggest that probiotics aren’t a one-size-fits-all therapy. A probiotic that provides relief to one person could evolve to become ineffective or even harmful in another. Probiotics have been linked to serious infections in some people.
“If we’re going to use living things as medicines, we need to recognize that they’re going to adapt, and that means that what you put in your body is not necessarily what’s going to be there even a couple hours later,” said senior author Gautam Dantas, professor of pathology and immunology, of molecular microbiology, and of biomedical engineering. “There is no microbe out there that is immune to evolution. This isn’t a reason not to develop probiotic-based therapies, but it is a reason to make sure we understand how they change and under what conditions.”
Everyone hosts a vast community of bacteria, viruses and fungi known as the gut microbiome in their digestive tracts. A well-balanced microbiome supplies us with vitamins, helps digest food, regulates inflammation and keeps disease-causing microbes in check. Probiotics in foods and dietary supplements are marketed as ways to keep healthy bacteria plentiful and digestion running smoothly.
They also are being developed as treatments for serious medical conditions such as inflammatory bowel disease; phenylketonuria (PKU), a metabolic disorder that causes neurological damage; and necrotizing enterocolitis, a life-threatening intestinal infection that affects premature babies. Like any other medication, a probiotic-based treatment must be proven safe and effective before the FDA will approve it for use in people. But when the therapy is a living thing that can change after it is administered, proving safety and efficacy poses special problems.
Understanding the principles that govern evolution in the digestive tract is a key step toward creating safe and effective probiotic therapeutics, the researchers said. Dantas and colleagues, including first authors Aura Ferreiro, a graduate student, and Nathan Crook, PhD, a former postdoctoral researcher in Dantas’ lab, turned to a probiotic known as E. coli Nissle 1917. The strain was isolated more than a century ago from a World War I soldier who emerged unscathed from an epidemic of severe diarrheal disease that sickened his comrades.
To study how the probiotic responds to different microbial communities, the researchers used mice that harbored four kinds of gut microbiomes: one with no pre-existing bacteria; another with a limited set of bacteria, characteristic of an unhealthy gut; a normal microbiome; and a normal microbiome after antibiotic treatment. The researchers gave the mice the probiotic, and then varied the food the mice ate, giving them either mouse chow, high-fiber pellets that mimic the natural mouse diet; high-fat, high-sugar, low-fiber pellets meant to model typical Western eating habits; and Western pellets plus fiber. After five weeks, the researchers obtained the bacteria from the mice’s guts and analyzed the microbes’ DNA.
“In a healthy, high-diversity background we didn’t capture a lot of adaptation, maybe because this is the background that Nissle is used to,” Ferreiro said. “But you have to remember that quite often we wouldn’t be using probiotics in people with a healthy microbiome. We’d be using them in sick people who have a low-diversity, unhealthy microbiome. And that seems to be the condition when the probiotic is most likely to evolve.”
Dantas and his colleagues applied these findings to designing a potential probiotic therapy for PKU. People with PKU are unable to break down phenylalanine, a protein building block found in many foods. High phenylalanine levels cause brain damage, so people with PKU must strictly adhere to a low-protein diet.
The researchers inserted a gene into Nissle that gave the bacteria the ability to degrade phenylalanine into a compound that is safely excreted in the urine. Then, they gave the bio-engineered bacteria to mice that lacked the capacity to metabolize phenylalanine. The next day, phenylalanine levels in some of the mice had dropped by half.
Moreover, the researchers did not find significant changes to the DNA of the engineered strain after one week of treatment, suggesting Nissle might be safe to use as a chassis for probiotic therapies over short time scales.
The finding that probiotics evolve and behave differently in individuals with disparate microbiomes and diets opens up avenues for personalizing probiotic-based medicine.
“Evolution is a given. Everything is going to evolve,” Dantas said. “We don’t need to be scared of it. We can use the principles of evolution to design a better therapeutic that is carefully tailored to the people who need it. This is an opportunity, not a problem.”