Three researchers at Washington University in St. Louis have received prestigious and highly competitive awards through the National Institutes of Health (NIH) Director’s High-Risk, High-Reward Research program. The awards support unconventional approaches to major challenges in biomedical and behavioral research.
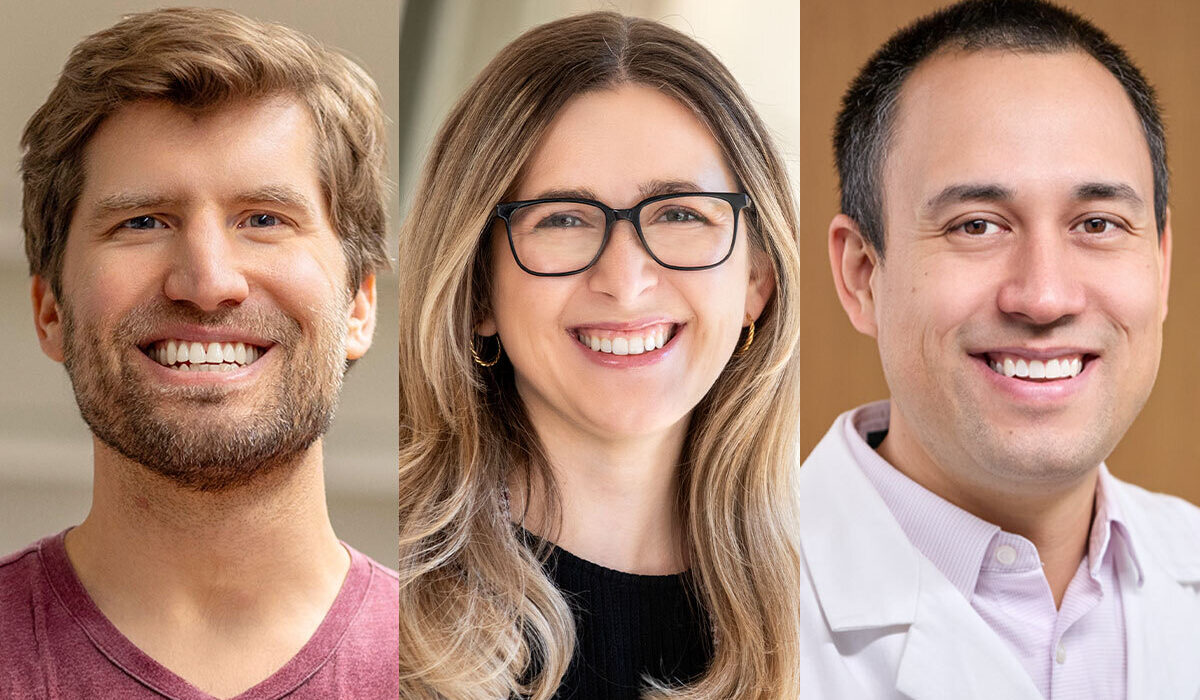
Michael P. Meers, PhD, has received the NIH Director’s New Innovator Award. Janet Sorrells, PhD, and Andrew L. Young, MD, PhD, have received the NIH Director’s Early Independence Award. The New Innovator Award supports unusually innovative research from investigators who are within 10 years of their final degree or clinical residency and have not yet received a large independent NIH grant. The Early Independence Award supports the launch of research careers for exceptional junior scientists who recently received their doctoral degree or completed clinical training.
Boosting the efficiency of regenerating tissue
Meers, an assistant professor in the Department of Genetics at WashU Medicine, is focused on developing new tools and techniques to help guide stem cells to becoming specific mature cell types. Such tools could nurture the nascent field of regenerative medicine, in which stem cells or even specialized cell types, such as skin cells, could be reprogrammed to form new tissues and organs that could replace those damaged by disease or injury.
Most existing processes for directing cells to take on particular functions or identities are inefficient in producing the targeted cell type, making them unsuitable to treating human disease. Meers and his team are developing a novel time-lapse profiling method to monitor changes in how a cell’s genes are regulated as it goes through the reprogramming process. A better understanding of these changes could lead to the development of more precise and efficient cell conversion methods that are more suitable for human therapeutics.
“Some of the most groundbreaking, paradigm-shifting science has historically come from the sorts of research that took risks, and we’re pleased to have the opportunity to pursue that sort of research with this NIH support,” Meers said. “This award is a green light to focus solely and without distraction on exactly what we think will make the greatest positive impact on scientific knowledge and human health.”
Revealing the origins of inflammatory bowel disease
Sorrells, an assistant professor in the Preston M. Green Department of Electrical & Systems Engineering at the McKelvey School of Engineering, is focused on developing a new imaging tool to study inflammatory bowel disease (IBD), a chronic gastrointestinal disorder that increases the risk of colorectal cancer. Significant gaps exist in the knowledge of how host cells and intestinal microbes interact in real time within the intestinal microenvironment.
Sorrells is developing an integrated optical imaging platform that can observe the intestinal microenvironment in mice with unprecedented spatial and temporal resolution. Most laboratory methods rely on bulk analysis of extracted tissue, which eliminates spatial context, or use imaging techniques that cannot achieve both the resolution and the speed needed to capture microbial behavior and host metabolism in vivo.
“We lose the ability to look at complicated dynamics that happen on the seconds scale within biological systems, and we also lose the ability to get higher throughput of larger areas,” she said. “One of the goals of this grant is to develop a new method for label-free super-resolution, with nonlinear optical microscopy.”
Sorrells’ approach ensures that the measurements reflect native physiology rather than an experimental artifact.
“The application is to look at a living gut microbiome,” she said. “Seeing how both bacteria and host cells are interacting over time and looking at how that changes spatially will help us better understand the many factors at play in the gut microbiome. Looking at live bacteria-host interactions will allow us to understand healthy and diseased states.”
The new imaging tool also could be used to study other complex tissue microenvironments, including those relevant to cancer, infection and autoimmune disorders.
Understanding aging’s effect on cancer risk
Young, an assistant professor in the Division of Hematology at WashU Medicine, studies how genetic mutations in blood and bone marrow cells acquired with age contribute to cancer risk. Most previous work in this area has looked at mutations in individuals who have already developed cancer, to see which mutations might have been responsible. Young’s research will focus on studying such mutations in cancer-free adults at advanced ages to better understand who goes on to develop cancer and why.
Because most of these cancer-related mutations can exist in the body for long periods of time but never lead to cancer, studying such genetic changes in healthy adults could provide new clues to preventing cancer.
“We have a relatively good understanding of how germline genetic risk, such as inherited BCRA1 mutations, and environmental exposures such as smoking lead to disease,” said Young, who treats patients at Siteman Cancer Center, based at Barnes-Jewish Hospital and WashU Medicine. “But we know less about how the genomic changes associated with ‘normal’ aging drive the development of disease and could be used to predict or prevent those diseases. This support will allow us to conduct the foundational experiments necessary to understanding how aging affects our bodies at the genomic level and how those genomic changes influence human disease.”
This work is supported by NIH grant numbers DP2 GM164659-01 (Meers), DP5 OD038607-01 (Sorrells) and DP5 OD039424-01 (Young). This work is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
About Washington University School of Medicine
WashU Medicine is a global leader in academic medicine, including biomedical research, patient care and educational programs with more than 3,000 faculty. Its National Institutes of Health (NIH) research funding portfolio is the second largest among U.S. medical schools and has grown 83% since 2016. Together with institutional investment, WashU Medicine commits well over $1 billion annually to basic and clinical research innovation and training. Its faculty practice is consistently among the top five in the country, with more than 2,000 faculty physicians practicing at 130 locations. WashU Medicine physicians exclusively staff Barnes-Jewish and St. Louis Children’s hospitals — the academic hospitals of BJC HealthCare — and Siteman Cancer Center, a partnership between BJC HealthCare and WashU Medicine and the only National Cancer Institute-designated comprehensive cancer center in Missouri. WashU Medicine physicians also treat patients at BJC’s community hospitals in our region. With a storied history in MD/PhD training, WashU Medicine recently dedicated $100 million to scholarships and curriculum renewal for its medical students, and is home to top-notch training programs in every medical subspecialty as well as physical therapy, occupational therapy, and audiology and communications sciences.
Originally published on the WashU Medicine website