What if a vaccine could protect people against all potentially deadly coronaviruses before one of them started the next pandemic?
Researchers at Washington University School of Medicine in St. Louis are working to reduce the risk of another devastating coronavirus pandemic by creating what is known as a pan-coronavirus vaccine. Such a vaccine is designed to reduce sickness and death resulting from the virus that causes COVID-19 as well as any other coronaviruses of concern, including ones that have not yet affected people. The research is supported by an $8 million grant from the National Institute for Allergy and Infectious Diseases of the National Institutes of Health (NIH).
There are good reasons to be prepared. Three times in the past two decades a coronavirus has emerged to sicken and kill people around the world. The severe acute respiratory syndrome (SARS) outbreak of 2003 killed 774 people. Middle East respiratory syndrome (MERS) coronavirus emerged in 2012 and has killed just under 1,000 people to date. The official death toll of the ongoing COVID-19 global pandemic is about 7 million, but the true total could be 15 million or more. And there’s no reason another coronavirus couldn’t emerge to threaten people again.
“Some coronaviruses that circulate in animals are just a few mutations away from having pandemic potential,” said co-principal investigator Michael S. Diamond, MD, PhD, the Herbert S. Gasser Professor of Medicine and a professor of molecular microbiology, and of pathology and immunology. “This is a significant concern. We know some of them already can infect human cells, they just lack the ability to be efficiently transmitted between people.”
The coronavirus family is enormous, and members of the family are unusually adept at infecting a wide variety of mammals and birds. The coronaviruses that sicken people originate in bats, which harbor at least 400 different strains, but they may infect other species before they get to people. The researchers are targeting their efforts to a subgroup known as betacoronaviruses because all of the strains most dangerous to people — the SARS, MERS and COVID-19 viruses — belong to that group. But even the known members of that subset represent a large and diverse group, and no doubt there are many more betacoronaviruses in wild animals that have not yet been encountered or studied.
Given what we don’t know and can’t know about the true extent of the coronavirus family, it is unrealistic to expect a pan-coronavirus vaccine to completely prevent severe illness and death, said Diamond and co-principal investigator Sean Whelan, PhD, the Marvin A. Brennecke Distinguished Professor and head of the Department of Molecular Microbiology. Instead, the goal is to create a vaccine capable of reducing sickness and death, and of inducing enough immunity in the population to slow the spread of disease. Such a vaccine could save countless lives by buying time for scientists to develop a targeted vaccine aimed at the specific strain of concern before an outbreak snowballs into a pandemic.
The task of creating a broadly protective vaccine is made more difficult by coronaviruses’ tendency to spin off new variants.
“One thing we’ve learned during the COVID-19 pandemic is that coronaviruses are very good at evading the immune response,” Whelan said. “We had amazingly good vaccines, and then variants started arising, and now we need boosters. It would be far better if we could find the parts of the virus that don’t mutate much, and use them to make a single vaccine that works broadly against all coronaviruses, even those we haven’t seen yet but may be coming.”
Diamond, Whelan and other Washington University researchers took part in the global race to create vaccines for COVID-19 that began in the early days of the pandemic. One of the experimental COVID-19 vaccines created at Washington University went on to prove effective in clinical trials and has been approved for use in India. It also has been licensed to the biotechnology company Ocugen with the aim of seeking approval in the United States and other countries.
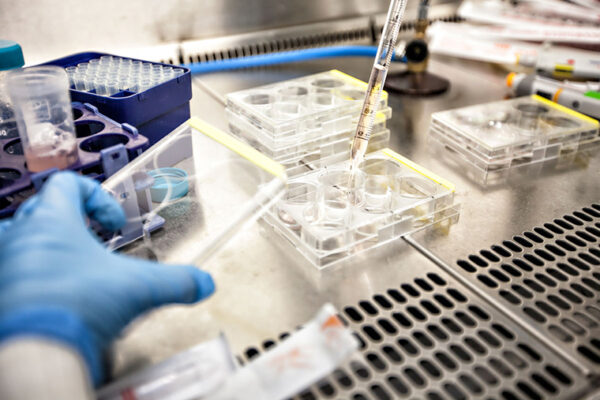
To design a pan-coronavirus vaccine, the research team first aims to identify parts of coronaviruses that remain consistent across the family, and then determine which of these viral regions elicit a strong and protective immune response. The team plans to target both the antibody response, which is important for reducing infection and transmission, and the cellular response, which is crucial for preventing severe disease and death. A group including Washington University researchers Ali Ellebedy, PhD, an associate professor of pathology and immunology, of medicine and of molecular microbiology; and Daved Fremont, PhD, a professor of pathology and immunology, of biochemistry and molecular biophysics and of molecular microbiology; is designing and evaluating molecules based on shared coronavirus features to elicit a strong antibody response. A second group led by Alba Grifoni, PhD, and Alessandro Sette, PhD, of the La Jolla Institute for Immunology, is working on identifying molecules to optimize the cellular immune response.
Once the first two groups have identified promising candidate molecules, a third group including Diamond and Whelan will insert the candidate molecules into harmless viruses to create experimental live-virus vaccines. Then, the researchers will first evaluate the experimental vaccines in mice and hamsters, looking closely at the strength and breadth of the immune response. Jacco Boon, PhD, an associate professor of medicine, of molecular microbiology and of pathology and immunology at Washington University, and Matthew Frieman, PhD, of the University of Maryland, Baltimore, will assess how well vaccination protects mice and hamsters from a variety of authentic coronaviruses.
“I fully expect that by the end of this process we will have at least one, maybe multiple, good candidates for a pan-coronavirus vaccine,” Diamond said. “The goal is to have a vaccine on hand that would limit severe disease and death in the case of an emerging coronavirus pandemic. That would buy us some time to create a more targeted vaccine and specific therapies to cut the pandemic short. It’s a big challenge, but I think this is something we can — and we must — achieve.”
Along with the researchers named above, the team also includes Galit Alter, PhD, and Aaron Schmidt, PhD, of Massachusetts General Hospital; Richard Scheuermann, PhD, of the J. Craig Venter Institute; and Bjoern Peters, PhD, and Daniela Weiskopf, PhD, of the La Jolla Institute for Immunology.
About Washington University School of Medicine
WashU Medicine is a global leader in academic medicine, including biomedical research, patient care and educational programs with 2,800 faculty. Its National Institutes of Health (NIH) research funding portfolio is the third largest among U.S. medical schools, has grown 52% in the last six years, and, together with institutional investment, WashU Medicine commits well over $1 billion annually to basic and clinical research innovation and training. Its faculty practice is consistently within the top five in the country, with more than 1,800 faculty physicians practicing at 65 locations and who are also the medical staffs of Barnes-Jewish and St. Louis Children’s hospitals of BJC HealthCare. WashU Medicine has a storied history in MD/PhD training, recently dedicated $100 million to scholarships and curriculum renewal for its medical students, and is home to top-notch training programs in every medical subspecialty as well as physical therapy, occupational therapy, and audiology and communications sciences.