Many young children who get a severe skin rash develop asthma months or years later. Doctors call the progression from eczema, or atopic dermatitis, to breathing problems the atopic march.
Now scientists at Washington University School of Medicine in St. Louis have uncovered what might be the key to atopic march. They’ve shown that a substance secreted by damaged skin circulates through the body and triggers asthmatic symptoms in allergen-exposed laboratory mice.
The findings, published May 19, 2009, in Public Library of Science Biology, suggest that early treatment of skin rash and inhibition of the trigger substance might block asthma development in young patients with eczema.
Fifty percent to 70 percent of children with severe atopic dermatitis go on to develop asthma, studies show. By comparison, the rate of asthma incidence among the general population is only about 9 percent in children and 7 percent in adults. Seventeen percent of U.S. children suffer from atopic dermatitis, although not all cases are considered severe.
“Over the years, the clinical community has struggled to explain atopic march,” says study author Raphael Kopan, Ph.D., professor of developmental biology and of dermatology. “So when we found that the skin of mice with an eczema-like condition produced a substance previously implicated in asthma, we decided to investigate further. We found that the mice also suffered from asthma-like responses to inhaled allergens, implicating the substance, called TSLP, as the link between eczema and asthma.”
Doctors and scientists had come up with theories to explain why a skin rash is sometimes associated with asthma. Do some people have an immune system disorder that causes an overreaction to allergens that contact the skin and lung airways? Or is it the opposite — do they have defective skin and airways that trigger an excessive immune response?
Kopan’s findings suggest the problem starts with damaged or defective skin. The researchers found that cells in damaged skin can secrete TSLP (thymic stromal lymphopoietin), a compound capable of eliciting a powerful immune response. And because the skin is so effective in secreting TSLP into the blood system, the substance travels throughout the body. When it reaches the lungs, it triggers the hypersensitivity characteristic of asthma.
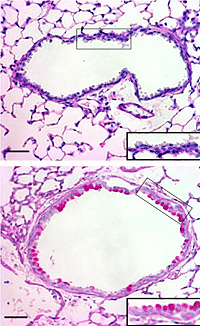
Led by doctoral student Shadmehr (Shawn) Demehri, the researchers studied mice that had been engineered with a genetic defect in patches of their skin. In the affected areas, the typically ordered layers of skin cells were disrupted, creating a condition similar to eczema. These patches were thickened and inflamed. The defective skin secreted TSLP as part of an alarm system alerting the body that its protective barrier function has failed — the substance activates an immune response that fights invaders.
Operating on the assumption that other barrier organs such as the lung will understand this alarm, the researchers tested what happened when the mice with skin defects inhaled an allergen. They found that their lungs reacted strongly — their breathing became labored and their lung tissue took on the traits that mark asthma in humans: mucous secretion, airway muscle contraction, invasion by white blood cells and conversion of lung cells from one type to another. Additional experiments showed that mice that had normal skin but were engineered to overproduce TSLP also developed the asthma-like symptoms.
“We are excited because we’ve narrowed down the problem of atopic march to one molecule,” Kopan says. “We’ve shown that skin can act as a signaling organ and drive allergic inflammation in the lung by releasing TSLP. Now it will be important to address how to prevent defective skin from producing TSLP. If that can be done, the link between eczema and asthma could be broken.”
TSLP is also produced in lungs of asthma patients, and Kopan says that research in the skin could eventually lead to ways to interfere with TSLP made in the lungs and thereby ease asthma development even in cases that aren’t linked to eczema.
“This research is a great example of the value of basic research approaches in uncovering the root causes of disease,” says Richard Anderson, M.D., Ph.D., of the National Institutes of Health’s National Institute of General Medical Sciences, which partially supported the work. “If these mechanisms operate the same way in humans, we could be on our way toward developing new strategies for preventing or treating asthma.”
Demehri S, Morimoto M, Holtzman MJ, Kopan R. Skin-derived TSLP triggers progression from epidermal-barrier defects to asthma. Public Library of Science Biology. May 19, 2009.
Funding from the National Institute of General Medical Sciences, Washington University, the Toyobo Biotechnology Foundation Long-term Research Grant and the Japanese Society for the Promotion of Science supported this research.
Washington University School of Medicine’s 2,100 employed and volunteer faculty physicians also are the medical staff of Barnes-Jewish and St. Louis Children’s hospitals. The School of Medicine is one of the leading medical research, teaching and patient care institutions in the nation, currently ranked third in the nation by U.S. News & World Report. Through its affiliations with Barnes-Jewish and St. Louis Children’s hospitals, the School of Medicine is linked to BJC HealthCare.


