An unexpected finding turned out to be a clue leading researchers at Washington University School of Medicine in St. Louis to propose a new treatment approach for Niemann-Pick disease, a rare, deadly neurodegenerative disorder.
To overcome the genetic defect in Niemann-Pick disease, the researchers suggest that chemical compounds could potentially “chaperone” mutant protein molecules through the cell’s quality control machinery. And they believe the approach also could be useful for more common diseases — such as cystic fibrosis — that stem from a similar type of defect.
Their findings are reported in advance online publication in the Journal of Biological Chemistry.
Daniel S. Ory, M.D., associate professor of medicine, and colleagues in the Center for Cardiovascular Research originally began to study Niemann-Pick type C disease because of its link to cholesterol metabolism — the genetic abnormality at the root of the disease serves as a tool for investigating how cholesterol moves about in cells.
Niemann-Pick type C, the rarest form of Niemann-Pick disease, usually affects school-aged children, but the disease may occur at any time from early infancy to adulthood. Symptoms may include unsteadiness of gait, clumsiness, slurred speech, learning difficulties, progressive intellectual decline, seizures and tremors. Niemann-Pick type C disease is fatal, and no life-extending treatment exists.
As the result of their latest research, Ory and colleagues want to follow up with an investigation of a different treatment modality than has previously been proposed. Prior avenues of treatment research emphasized using gene therapy to repair the genetic defect, but such an approach is fraught with numerous difficulties. Ory’s group believes that Niemann-Pick type C and other diseases like it might be treated more readily with chemical compounds able to compensate for the effect of the disease’s underlying genetic mutation.
Niemann-Pick type C disease is a recessive inherited trait that can originate in one of more than 200 different mutations in the NPC1 gene, which lies on chromosome 18. The mutations lead to production of abnormal NPC1 protein. Normally, NPC1 protein plays an essential role in moving cholesterol out of cells, and if it doesn’t function, cholesterol and other lipids accumulate.
Most scientists assumed that Niemann-Pick type C mutations produced NPC1 protein that didn’t work correctly. So when a routine test in the Ory lab of a mutated NPC1 protein showed that the protein was in fact active in living cells, the researchers did a double take.
“It is unequivocal that the mutation causes disease in human patients,” says Ory, also associate professor of cell biology and physiology. “Yet the mutated protein seemed functional when we introduced it into cells.”
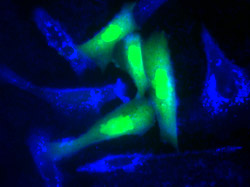
When they looked for the explanation for this aberration, Ory and colleagues found that a small proportion of the mutant protein actually could do the job of normal NPC1 protein. It turned out that the mutation caused most newly minted NPC1 protein molecules to fold into the wrong shape or to assume their final shape slowly so that the cell’s quality control checkpoints rejected them. But some of the mutant protein molecules assumed the correct shape and made it to their proper destination.
That suggested to the team that Niemann-Pick type C disease possibly could be treated with chemicals that assist the mutant proteins produced in patients. Ory refers to these as chemical chaperones and indicates this approach could help the large NPC1 proteins during the process of folding their long, complex chains so that more of the mutant proteins fold properly and pass through the cell’s quality control checkpoints.
In collaboration with the National Institutes of Health Chemical Genomics Center, Ory will next screen more than 200,000 compounds to see which ones increase the amount of mutant NPC1 that folds into a functional form.
“The screening can be done in as little as two weeks because the facility in Rockville, Md., has a huge library of compounds and state-of-the-art robotic equipment that can perform the tests at very high speed,” Ory explains. “Then we will bring the compounds that show a positive effect to our laboratory and validate them on cell lines from Niemann-Pick patients. After that we will work with a pharmaceutical partner to take the ones that are effective in cells and make sure they will be safe and effective in people.”
Although Niemann-Pick disorders are rare, affecting fewer than 2,000 people worldwide, Ory says that it is likely the chemical chaperone approach to therapy could also be useful for other disorders caused by genetic mutations that lead to protein misfolding. This includes cystic fibrosis, a lung and digestive system disorder that affects 70,000 children and adults around the world.
Gelsthorpe ME, Baumann N, Millard E, Gale SE, Langmade SJ, Schaffer JE, Ory DS. NPC1 I106T mutant encodes a functional protein that is selected for ER-associated degradation due to protein misfolding. Journal of Biological Chemistry Jan. 23, 2008 (advance online publication).
Funding from the National Institutes of Health and the Ara Parseghian Medical Research Foundation supported this research.
Washington University School of Medicine’s 2,100 employed and volunteer faculty physicians also are the medical staff of Barnes-Jewish and St. Louis Children’s hospitals. The School of Medicine is one of the leading medical research, teaching and patient care institutions in the nation, currently ranked fourth in the nation by U.S. News & World Report. Through its affiliations with Barnes-Jewish and St. Louis Children’s hospitals, the School of Medicine is linked to BJC HealthCare.