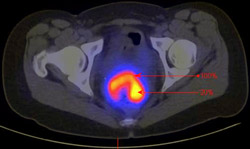
It doesn’t matter how small or large it is, if a cervical tumor glows brightly in a PET scan, it’s apt to be more dangerous than dimmer tumors. That’s the conclusion of a new study of cervical cancer patients at Washington University School of Medicine in St. Louis.
 |
|
Elizabeth Kidd discusses the results of the study.
|
|
|
“We’ve seen that among patients with the same stage of cervical cancer, there will be some patients who don’t respond to treatment as well as others,” says lead author Elizabeth A. Kidd, M.D., a Barnes-Jewish Hospital resident in Washington University’s Department of Radiation Oncology. “Our study suggests that PET (positron emission tomography) can reliably identify patients who have a poorer prognosis.”
Kidd and her colleagues, including researchers with the Siteman Cancer Center at Washington University and Barnes-Jewish Hospital, report their findings in an upcoming issue of the journal Cancer.
The researchers used FDG-PET, a widely available three-dimensional scanning technique. FDG-PET measures how rapidly tumors take up a radiolabeled glucose tracer (FDG) — high uptake results in a stronger or brighter signal in the scan. The researchers found that the higher the standard uptake value (SUV) for FDG in the primary tumor, the greater the recurrence rate and the lower the survival rate of patients.
“FDG-PET is the most commonly used PET scan,” Kidd explains. “It’s standard for patients to have this type of scan once diagnosed with cervical cancer. Oncologists use it to see the extent of the primary tumor and to look for tumors that have spread beyond the pelvis. But this study shows that the SUV obtained from FDG-PET can also tell physicians how well a patient will respond to treatment and should be part of the evaluation process.”
A high SUV at diagnosis could signal that a patient should be followed more closely than usual after treatment to catch recurrences earlier, according to Kidd. She also indicates that although the results suggest that patients with high SUV tumors may need more aggressive treatments, further clinical studies will be necessary to determine the best therapy in such cases.
In the current study, 287 patients with cervical cancer were treated with surgery, chemotherapy or radiation therapy following standard treatment protocols. At the time of diagnosis, the SUV of their primary tumor was obtained. Their cancers were also staged under standard guidelines, which rely largely on tumor size and involvement with surrounding tissues. The patients’ cancers ranged from early (stage 1A2) to highly advanced (stage 4B).
The researchers showed that patients who had a high tumor SUV were more likely to have aggressive disease: They were likely to have cancerous cells in their lymph nodes, persistent disease after initial treatment, recurrence of disease in the pelvis and lower survival rates. They also found that tumor SUV did not depend on the tumor stage or volume — large tumors could have a relatively low SUV, and small tumors could have a high SUV.
The findings suggest that SUV is a more sensitive indicator of tumor aggressiveness than standard staging protocols. The study also demonstrated that SUV was better at predicting overall survival than the type of tumor or lymph node involvement, factors suspected to affect prognosis.
The patients were found to fall into three distinct risk groups. Those with the lowest SUV had a survival rate of 95 percent at five years, those in the middle SUV range had a 70 percent five-year survival rate, and those in the highest SUV range had a 44 percent five-year survival rate.
Because high SUV indicates that tumors take up glucose rapidly, the measurement may point to an important biological difference in these more aggressive cancers. “We’re interested in finding out what causes that difference,” Kidd says. “That could eventually lead to new methods for treating patients whose tumors have a high SUV.”
Kidd presented the study’s findings in Amsterdam in May at the meeting of the American Radium Society, the oldest society devoted to the study and treatment of cancer. The society gave Kidd one of three 2007 Young Oncologist Essay Awards and funded her travel to the conference.
Kidd EA, Siegel BA, Dehdashti F, Grigsby PW. The standardized uptake value for F-18 fluorodeoxyglucose is a sensitive predictive biomarker for cervical cancer treatment response and survival. Cancer, Sept. 4, 2007 (advance online publication).
Washington University School of Medicine’s full-time and volunteer faculty physicians also are the medical staff of Barnes-Jewish and St. Louis Children’s hospitals. The School of Medicine is one of the leading medical research, teaching and patient care institutions in the nation, currently ranked fourth in the nation by U.S. News & World Report. Through its affiliations with Barnes-Jewish and St. Louis Children’s hospitals, the School of Medicine is linked to BJC HealthCare.
Siteman Cancer Center is the only NCI-designated Comprehensive Cancer Center within a 240-mile radius of St. Louis. Siteman Cancer Center is composed of the combined cancer research and treatment programs of Barnes-Jewish Hospital and Washington University School of Medicine.