About 30 first- and second-year School of Medicine students got hands-on medical experience during recent spring-break trips to a Navajo reservation and Nicaragua.
The Forum for International Health and Tropical Medicine (FIHTM), a student group that works to expose the medical community firsthand to international health concerns, sponsored the trips. In addition to receiving money from the medical school for the trips, the group raised about $2,000 through bake sales, a pasta dinner and a raffle. Area physicians, clubs and churches donated medications and medical supplies.
Eighteen first-year students spent a week in the Teec Nos Pos region of the Navajo Nation in northeastern Arizona teaching elementary, middle- and high-school students about aspects of health care relevant to the culture and observing the health-care system.
Michelle Sabo, a first-year medical student, said the group spent several days teaching the pupils about obesity and diabetes, a major health problem for American Indians. They played games with the younger children to instill the importance of exercise and proper nutrition. They also talked with older children about why alcohol and tobacco are unhealthy.
All 18 students bunked in the living room of a reservation youth worker’s small home, which was stressful, Sabo said, but the overall trip was a worthwhile experience that taught them a lot about the life of American Indians.
“I learned a lot about public health and about a whole different culture within our country’s boundaries,” Sabo said. “I also learned about myself in situations of stress, which was as important as working with the kids.
“We’re going to be doctors in a lot of high-stress situations. The more we are exposed to those situations and learn how to deal with them, the better off we are,” Sabo said.
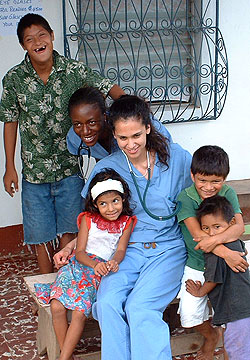
Under supervision of physicians with International Service Learning, the second-year students provided health care in Nicaragua to those who don’t have access to it. They took with them 11 duffel bags of medical supplies and medications.
Shada Rouhani, a second-year student who coordinated the trip, said the experience was “eye opening.
“We saw a number of medical conditions that we don’t see in the United States,” she said. “We saw people in unfortunate situations handling problems that you’d hope they wouldn’t have to deal with.”
The 11 second-year students went house-to-house in Pearl Lagoon and Bluefields, on the Atlantic coast of the Central American country, talking with residents and determining health-care needs. For those who needed diagnosis and treatment, the students gave them appointments to go to a clinic the next day. Patients could also come without an appointment.
On the morning the students arrived to work in the clinic in Pearl Lagoon, there were 200 patients waiting to be seen, Rouhani said. The group was only able to see about half of the patients, many of whom had infectious diseases, pneumonia, complications of diabetes and high blood pressure, and infections, among other issues.
“It was frustrating because if they lived in the United States, these things could be treated easily,” Rouhani said. “For these patients, there is no treatment available locally, and even if there were, they couldn’t afford it.”
One patient was severely anemic and needed to be transported to another town where there was a hospital for a blood transfusion. However, the group learned that in Nicaragua, patients must bring blood with them for a transfusion or buy it from the hospital, which for many is much more than they can afford.
Rouhani said the trip was a good learning experience and strengthened her resolve to include international health in her future career plans.
“The learning curve in four days was unbelievable,” she said. “We learned things about diagnosis, treatment, health and socioeconomic conditions that we could never learn in the classroom.”