Tip sheets highlight timely news and events at Washington University in St. Louis. For more information on any of the stories below or for assistance in arranging interviews, please see the contact information listed with each story.
I don’t remember!
Alcohol-Induced blackouts may be genetic

More than 50,000 people in the United States are waiting for kidney transplants. Most are waiting for someone who wants to be an organ donor to die, but each year only 9,000 people on the transplant waiting list get a kidney from someone who has died, while 16,500 die. Transplants from living donors have the greatest chance of working for a long time and can happen quickly, often within a year. A living kidney donor may be a family member or friend between the ages of 18 and 65. They must be healthy and have a blood type that is compatible with the recipient’s blood type. But researchers at Washington University School of Medicine, have discovered something surprising. Many interested kidney donors are not taken up on their offers to donate because the recipients are afraid donors will be harmed. As a result, many potential donor kidneys go unused.
Unsuspected player in Alzheimer’s diagnosis
Finding could make it possible to diagnose and forecast risk for Alzheimer’s disease
Preliminary research suggests it may someday be possible to diagnose and forecast risk for Alzheimer’s disease using skin cells, thanks to a small protein, or peptide, that few previously associated with the disease. Researchers at Washington University School of Medicine in St. Louis have discovered that skin cells from people with inherited forms of Alzheimer’s disease respond to the peptide by triggering Alzheimer’s-like changes, but skin cells from healthy individuals do not. They say the findings need to be explored further in cases of non-inherited Alzheimer’s disease, but the results could eventually lead to a way of determining an individual’s risk of developing Alzheimer’s before clinical symptoms arise.
Not for pitchers only
Rotator cuff repair with smaller incisions and sturdier stitches
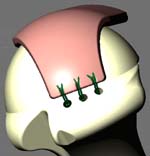
Each year in the United States, nearly 300,000 people have surgery to repair their rotator cuff. The rotator cuff is made up of several muscles that allow us to lift our arms or to rotate them during sports activities such as golf, tennis and swimming. The rotator cuff also is used during lifting, washing windows and working in the garden. In the past, surgical correction of the rotator cuff involved an incision through the deltoid muscle on the outside of the shoulder, a lot of pain for weeks after surgery and a long period of recovery. But Washington University orthopaedic surgeons have begun using a minimally invasive system that eliminates the need for the incision through the muscle and limits the amount of post-operative pain. The system allows surgeons to strengthen the repair with a suturing device that sews the muscle right into bone where it can heal more quickly, with less pain.