Approximately 9.5 million people globally live with Type 1 diabetes, a chronic autoimmune disease where T cells from the body’s immune system destroy insulin-producing cells in the pancreas, which are needed to control blood-sugar levels. Daily insulin injections and continual blood glucose monitoring help control the disease, but there is no cure or preventive.
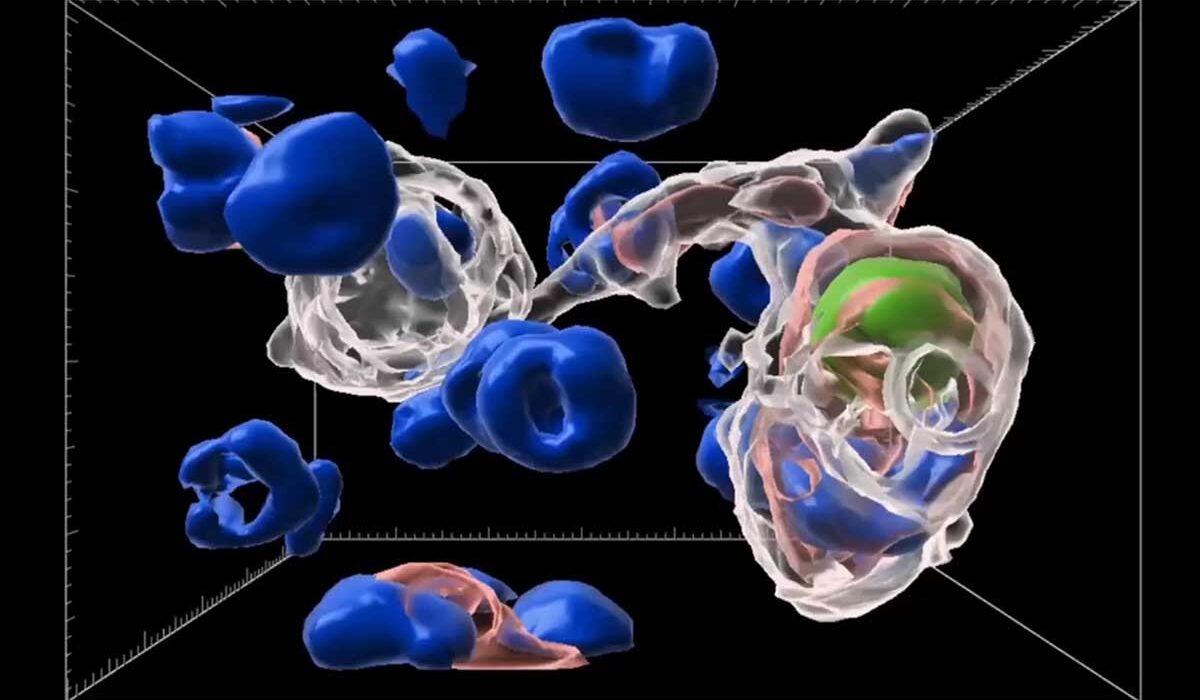
Now, researchers at Washington University School of Medicine in St. Louis have found a group of immune cells in the pancreas that can render T cells inactive, protecting insulin-producing beta cells and preventing Type 1 diabetes from developing in mice otherwise destined to develop the disease. The newly identified cells are a type of macrophage — immune cells that consume dead cells throughout the body to help keep tissue healthy.
The researchers revealed that the protective macrophages, which they dubbed efferocytic macrophages, or eMacs, acquired the ability to silence T cells after consuming dead cells in the pancreas.
The findings appear in Nature Oct. 1.
“Now we know the identity of the cells that can make T cells less responsive,” said senior author Kodi Ravichandran, PhD, the Robert L. Kroc Professor of Pathology & Immunology and a BJC Investigator at WashU Medicine. “If we can mimic the series of events responsible for converting macrophages into e-Macs, we could potentially boost them to help prevent or control Type 1 diabetes and even other autoimmune diseases.”
Garbage-engulfing immune cells protect
The pancreas contains clusters of cells called beta cells whose job is to produce insulin, a hormone that’s critical for keeping blood-sugar levels in a safe range. A small number of beta cells routinely die to reduce inflammation and keep tissues healthy, a natural process that happens in cells throughout the body.
Macrophages then engulf and digest the cellular debris in a process called efferocytosis. These garbage-eating cells also play an important role in influencing the behavior of T cells throughout the body. The researchers wondered if such macrophages play a role in helping to maintain the health of the pancreatic tissue by influencing the immune system.
“How macrophages engage and consume cellular garbage can influence what is happening in the cellular neighborhood,” said Ravichandran. “And this also guides how macrophages interact with T cells.”
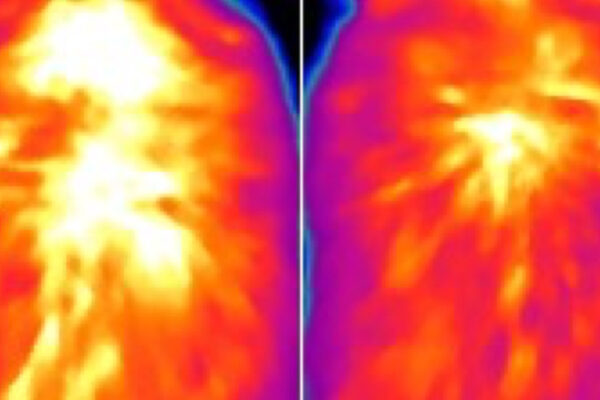
For example, macrophages can activate T cells to help fight an infection after consuming a dying infected cell. In the case of naturally dying beta cells in the pancreases of mice, the researchers found that after engulfing the cells, the eMacs shifted their behavior to deactivate T cells, protecting the surrounding healthy beta cells from attack. The researchers surmised that the macrophages essentially acquired this behavior after consuming the dead beta cells and that if this can be mimicked, then the healthy beta cells could be protected from attack by T cells in the context of diabetes.
In the study, the researchers administered a single low dose of a chemotherapy drug, streptozotocin, to mice prone to Type 1 diabetes in an experiment designed to kill a few cells in the pancreas, mimicking the natural process of cell death that happens in healthy people when maintaining the health of their organs. They found a greater proportion of e-Macs among the macrophages in the pancreases of mice treated with streptozotocin compared with those of mice given a placebo. Streptozotocin-treated mice were protected from developing diabetes for more than 40 weeks, while mice given the placebo became diabetic by 20 weeks and did not survive past 30 weeks.
The researchers hope to find ways to boost e-Macs in humans for therapeutic use, Ravichandran said. They also identified a subset of macrophage analogs to the mouse e-Macs in the pancreases of deceased human organ donors.
“Because these trash-disposing pancreatic macrophages become protective against Type 1 diabetes, we are intrigued by the possibility of leveraging their disease-preventing properties in people at high risk for this condition,” Ravichandran said.
Future studies aim to focus on increasing the fraction of e-Macs in the pancreas with the goal of helping people with a family history of Type 1 diabetes to prevent the disease.
Other WashU Medicine collaborators on the study included first author Pavel Zakharov, PhD, an instructor of pathology and immunology; Xiaoxiao Wan, MD, PhD, an assistant professor of pathology and immunology; Eynav Klechevsky, PhD, an associate professor of pathology and immunology; and the late Emil R. Unanue, PhD, who died before seeing the study’s completion. Unanue, a 1995 Albert Lasker Basic Medical Research Award winner, was a pioneer in describing the interactions between T cells and presenting cells — immune cells that display a sample of a potential threat on their surface – that make it possible for the former to recognize and respond to foreign invaders.
Zakharov PN, Chowdhury CS, Peterson OJ, Barron B, Vomund AN, Gorvel L, Unanue ER, Klechevsky E, Wan X, Ravichandran KS. Efferocytic remodeling of pancreatic intra-islet macrophages by limited β-cell death. Oct. 1, 2025. Nature. DOI: 10.1038/s41586-025-09560-4
This work was supported by the National Institute of Allergy and Infectious Diseases of the National Institutes of Health (NIH), grant number R01AI159551; and by the BJC Investigator Funds from WashU Medicine. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
About Washington University School of Medicine
WashU Medicine is a global leader in academic medicine, including biomedical research, patient care and educational programs with more than 3,000 faculty. Its National Institutes of Health (NIH) research funding portfolio is the second largest among U.S. medical schools and has grown 83% since 2016. Together with institutional investment, WashU Medicine commits well over $1 billion annually to basic and clinical research innovation and training. Its faculty practice is consistently among the top five in the country, with more than 2,000 faculty physicians practicing at 130 locations. WashU Medicine physicians exclusively staff Barnes-Jewish and St. Louis Children’s hospitals — the academic hospitals of BJC HealthCare — and Siteman Cancer Center, a partnership between BJC HealthCare and WashU Medicine and the only National Cancer Institute-designated comprehensive cancer center in Missouri. WashU Medicine physicians also treat patients at BJC’s community hospitals in our region. With a storied history in MD/PhD training, WashU Medicine recently dedicated $100 million to scholarships and curriculum renewal for its medical students, and is home to top-notch training programs in every medical subspecialty as well as physical therapy, occupational therapy, and audiology and communications sciences.
Originally published on the WashU Medicine website