A new technology that harnesses artificial intelligence (AI) to analyze mammograms and improve the accuracy of predicting a woman’s personalized five-year risk of developing breast cancer has received Breakthrough Device designation from the Food and Drug Administration (FDA). Developed by researchers at Washington University School of Medicine in St. Louis, the software has been licensed to Prognosia Inc., a WashU startup company.
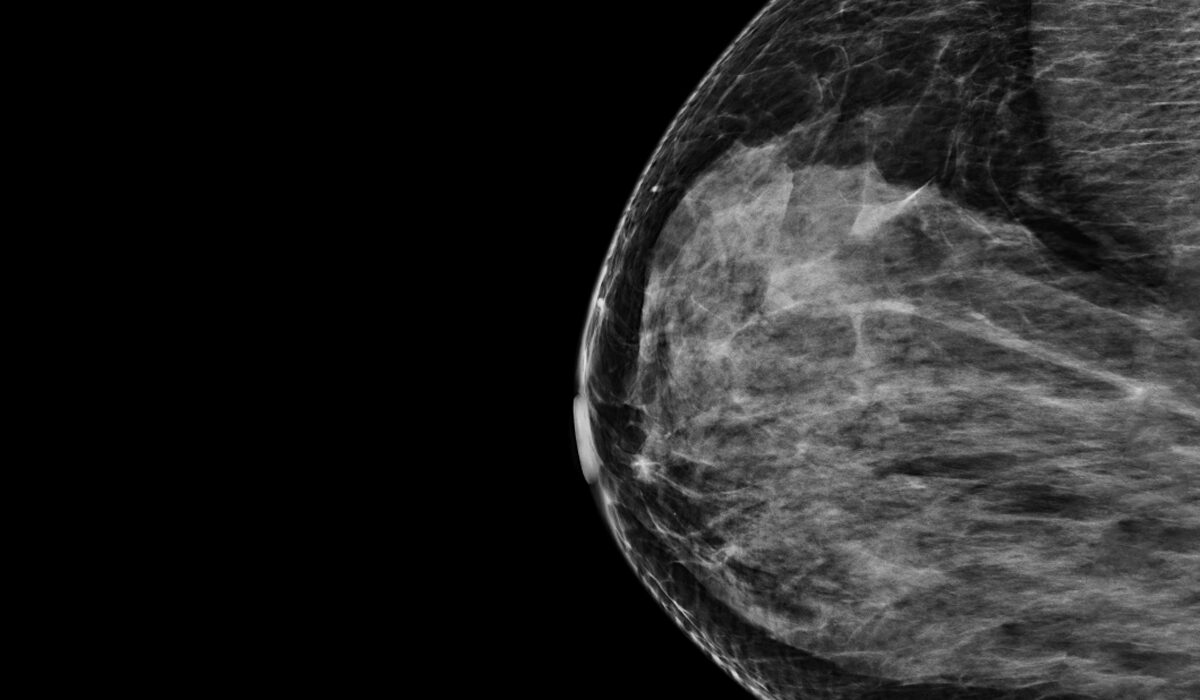
The system analyzes mammograms to produce a risk score estimating the likelihood that a woman will develop breast cancer over the next five years. The technology is compatible with both types of mammogram imaging available: the four 2D views of the breast produced by full-field digital mammography and the synthetic 3D view of the breast produced by digital breast tomosynthesis. Importantly, the system produces an absolute five-year risk that makes it possible to compare a woman’s risk to an average risk based on national breast cancer incidence rates. This provides a meaningful estimate that is aligned with the U.S. national risk reduction guidelines, so that clinicians will know what steps to take next if a woman’s risk is elevated.
The FDA Breakthrough Device designation provides an expedited review process for full market approval in an effort to give patients and clinicians accelerated access to new medical devices. Products that receive the designation have already undergone rigorous testing and shown excellent promise in their potential to improve treatment or the diagnosis of debilitating or life-threatening conditions.
The software package, called Prognosia Breast, was developed by Graham A. Colditz, MD, DrPH, the Niess-Gain Professor of Surgery at WashU Medicine and associate director of prevention and control at Siteman Cancer Center, based at Barnes-Jewish Hospital and WashU Medicine; and Shu (Joy) Jiang, PhD, an associate professor of surgery in the Division of Public Health Sciences in the Department of Surgery at WashU Medicine. Colditz and Jiang co-founded Prognosia in 2024 in collaboration with WashU’s Office of Technology Management (OTM) and BioGenerator Ventures, the latter of which provided both financial support and business strategy expertise from Entrepreneur-in-Residence David Smoller, PhD.

The software is a pre-trained machine learning system that analyzes mammogram images and provides an estimate of how likely a patient is to develop breast cancer over the next five years, based solely on images and a woman’s age. According to the developers, Prognosia Breast estimates a person’s five-year risk of developing breast cancer 2.2 times more accurately than the standard method, which is based on questionnaires that consider factors such as age, race and family history. The system was trained on past mammograms from tens of thousands of individuals who underwent breast cancer screening through Siteman Cancer Center. Some of them went on to develop cancer, teaching the system what to look for in the earliest stages of tumor development. Such early signs of disease can’t be perceived even by a well-trained human eye.
“We’re excited about the potential of this technology to improve risk prediction and prevention of breast cancer broadly, no matter where a woman is getting screened,” Colditz said. “The long-term goal is to make this technology available to any woman having a screening mammogram anywhere in the world. No matter the type of imaging they receive, our data show the software’s potential to identify women at increased risk of developing breast cancer over the next five years, providing them with opportunities to take targeted steps to reduce that risk.”
The new device could have a large impact on risk prediction because the infrastructure is already in place to begin immediately using the software anywhere mammography is provided. Furthermore, many women already receive regular mammograms. According to 2023 survey data from the Centers for Disease Control and Prevention, more than 75% of women ages 50 to 74 reported having received a mammogram in the past two years.
Even with widespread screening, about 34% of breast cancer patients in the U.S. are diagnosed at later stages of the disease. According to the investigators, being able to assess risk up to five years in advance of the onset of cancer is likely to improve early detection, reducing the number of late-stage cancers diagnosed. Early detection has been shown to make treatment more effective and reduce deaths from breast cancer.
“Receiving a Breakthrough Device designation is a powerful validation of the extraordinary dedication and vision of this research team to improve breast cancer diagnosis and care,” said Doug E. Frantz, PhD, vice chancellor for innovation and commercialization at WashU. “It takes years of concerted effort to produce software that could quickly be integrated into the workflow of any mammography center, significantly enhancing the clinical value of routine mammograms no matter where they are provided. This is a prime example of the vital role of entrepreneurship and commercialization at WashU in transforming cutting-edge research into real-world technologies that improve patient care.”
The device produces a five-year risk score that is intended to complement, not replace, the analysis provided by radiologists, who will continue to review the mammograms following standard protocols. According to the American Society of Clinical Oncology and the U.S. Preventive Services Task Force, a five-year risk score of 3% or higher is considered elevated. According to guidelines from these organizations, women with elevated scores should be referred to specialists who can further advise them on their options for additional screening and prevention strategies.
About one in eight women in the U.S. will be diagnosed with breast cancer in their lifetime. Those found to be at elevated risk of this cancer have the option to receive more frequent screening — which may include other types of imaging, such as MRI — and in some cases may choose to take a type of chemotherapy called tamoxifen or endocrine therapy as preventive treatments. With such options available, identifying women at high risk is important so they have access to specialists who can help guide them in making these important choices.
The developers are planning a clinical trial at Siteman Cancer Center that will apply the risk score from Prognosia Breast in combination with the standard mammography screening protocols. Standard screening protocols include the review of mammograms and measures of breast density already provided to all patients. Individuals found to be at elevated risk will be referred to Siteman’s breast health specialists, who focus on helping individuals navigate the options they have for managing high breast cancer risk.
“Despite the sophistication of today’s breast imaging and its broad use for identifying existing tumors, today’s risk prediction for breast cancer is still questionnaire-based and not very good at estimating future risk,” Jiang said. “Our work has focused on filling that need for better methods. Moving to image-based risk prediction — which our studies have shown is much more accurate — has the potential to be revolutionary for patient care.”
The current FDA designation applies to the software’s analysis of mammogram images taken at a single time point. In the future, the researchers plan to update Prognosia Breast to analyze several years of mammograms from the same individual, which may further improve the accuracy of the prediction.
About Washington University School of Medicine
WashU Medicine is a global leader in academic medicine, including biomedical research, patient care and educational programs with 2,900 faculty. Its National Institutes of Health (NIH) research funding portfolio is the second largest among U.S. medical schools and has grown 83% since 2016. Together with institutional investment, WashU Medicine commits well over $1 billion annually to basic and clinical research innovation and training. Its faculty practice is consistently within the top five in the country, with more than 1,900 faculty physicians practicing at 130 locations. WashU Medicine physicians exclusively staff Barnes-Jewish and St. Louis Children’s hospitals — the academic hospitals of BJC HealthCare — and treat patients at BJC’s community hospitals in our region. WashU Medicine has a storied history in MD/PhD training, recently dedicated $100 million to scholarships and curriculum renewal for its medical students, and is home to top-notch training programs in every medical subspecialty as well as physical therapy, occupational therapy, and audiology and communications sciences.
Originally published on the WashU Medicine website