An international phase 3 clinical trial led by Washington University School of Medicine in St. Louis and Dana-Farber Brigham Cancer Center shows that patients with certain locally advanced head and neck cancers benefited from the addition of the immunotherapy drug pembrolizumab (brand name Keytruda) to standard-of-care therapy. Patients who received pembrolizumab saw greater tumor shrinkage prior to surgery and, on average, survived cancer-free almost two years longer than did patients who only received standard-of-care therapy.
These results are reported April 27 at the annual meeting of the American Association for Cancer Research (AACR) in Chicago. WashU Medicine researchers co-led the study at Siteman Cancer Center, based at Barnes-Jewish Hospital and WashU Medicine.
In locally advanced head and neck cancers, the tumor has spread to nearby tissues or lymph nodes but has not yet metastasized to distant organs. Standard-of-care therapy for these patients includes surgery to remove the tumor followed by radiation given with or without chemotherapy. Only 40% to 50% of such patients are alive five years after standard-of-care therapy.
Pembrolizumab, a type of immunotherapy that helps a patient’s own immune system attack cancer cells, was first approved by the Food and Drug Administration (FDA) in 2014 for advanced melanoma. It has since been approved for many other cancers, including advanced lung cancer, colorectal cancer, cervical cancer and lymphoma. In 2016, it was approved for recurrent and metastatic head and neck cancer.
If approved for locally advanced head and neck cancers, which was the focus of the clinical trial, pembrolizumab — given before and after surgery to remove the tumor — will be the first change in standard-of-care therapy for this cancer type in more than two decades.
“The survival benefit we’ve seen in adding pembrolizumab to standard-of-care therapy for patients with locally advanced head and neck cancer is clinically meaningful and groundbreaking,” said co-senior author Douglas R. Adkins, MD, a professor of medicine and director of the Section of Head and Neck and Thyroid Medical Oncology at WashU Medicine. Adkins treats patients at the Robert Ebert and Greg Stubblefield Head & Neck Tumor Center at Siteman Cancer Center.
The proposal to evaluate pembrolizumab in this cancer type originated at WashU Medicine and formed the basis of an earlier phase 2 clinical trial that began at Siteman in 2013. The findings from that study led directly to this international phase 3 trial.
“It’s exciting to see our ideas move toward clinical practice with such impressive and potentially life-changing results,” Adkins added.
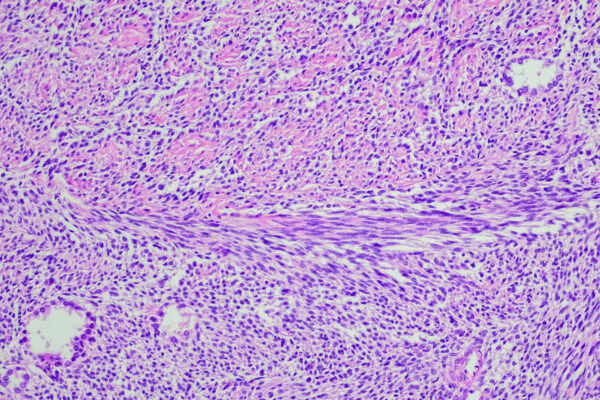
The new phase 3 study enrolled 714 patients with newly diagnosed stage III or stage IVA head and neck squamous cell carcinoma. Beginning in December 2018, patients were randomly assigned to receive standard-of-care therapy alone, which includes surgery and radiation given with or without chemotherapy, or to standard-of-care therapy plus pembrolizumab given before and after surgery.
Analyzing data collected through July 2024, patients who received standard-of-care therapy plus pembrolizumab survived cancer-free for a median of 51.8 months (about 4.3 years), compared with a median of 30.4 months (about 2.5 years) for those who received standard-of-care therapy alone. Those given pembrolizumab also experienced greater reductions in tumor size prior to surgery, an important outcome given that therapies that shrink a tumor before its removal may reduce the risk of the cancer returning later.
The phase 3 study, funded by Merck, builds upon the work started in 2013 by Adkins and Ravindra Uppaluri, MD, PhD, who was then with WashU Medicine and is now the director of Head and Neck Surgical Oncology at Dana-Farber and Brigham and Women’s Hospital. Adkins and Uppaluri proposed investigating whether giving pembrolizumab before and after surgery would improve outcomes for patients undergoing surgical removal of locally advanced head and neck cancers that have not yet become metastatic.
Merck also funded the earlier phase 2 trial, which found that adding pembrolizumab before and after surgery increased tumor cell death. The therapy was found to be safe and did not harm the delivery of standard-of-care therapy. After this therapy, the researchers found, patients’ cancers returned at lower rates than expected compared with historical data. This set the stage for the current phase 3 randomized trial that included more patients and a control group and was conducted at multiple sites around the world.
Pembrolizumab is what’s known as an immune checkpoint inhibitor, meaning that it works by skirting roadblocks that keep the body’s own immune cells from destroying tumor cells. One of these roadblocks is a protein on the surface of tumors called PD-L1. By circumventing PD-L1, pembrolizumab allows the patient’s own immune cells to attack and kill tumor cells.
Head and neck cancers include tumors of the mouth, sinuses, nose and throat. Smoking and other tobacco use as well as human papillomavirus (HPV) infection increase the risk of such cancers.
The FDA is scheduled to announce a decision on approving pembrolizumab for locally advanced head and neck cancers in June.
Uppaluri R, Haddad RI, Tao Y, Le Tourneau C, Lee NY, Westra W, Chernock R, Tahara M, Harrington K, Klochikhin AL, Brana I, Vasconcelos Alves G, Hughes BGM, Olivia M, Pinto Figueiredo Lima I, Ueda T, Rutkowski T, Schroeder U, Mauz P, Fuereder T, Laban S, Oridate N, Popovtzer A, Mach N, Korobko Y, Alpuim Costa D, Hooda-Nehra A, Rodriguez CP, Bell RB, Manschot C, Benjamin K, Gumuscu B, Adkins D. Neoadjuvant and adjuvant pembrolizumab plus standard of care in resectable locally advanced head and neck squamous cell carcinoma: phase 3 KEYNOTE-689 study. Advances in Immunotherapy, Clinical Trials Plenary Session. American Association for Cancer Research (AACR) Annual Meeting. April 27, 2025.
This research was funded by Merck Sharp & Dohme LLC.
About Washington University School of Medicine
WashU Medicine is a global leader in academic medicine, including biomedical research, patient care and educational programs with 2,900 faculty. Its National Institutes of Health (NIH) research funding portfolio is the second largest among U.S. medical schools and has grown 56% in the last seven years. Together with institutional investment, WashU Medicine commits well over $1 billion annually to basic and clinical research innovation and training. Its faculty practice is consistently within the top five in the country, with more than 1,900 faculty physicians practicing at 130 locations and who are also the medical staffs of Barnes-Jewish and St. Louis Children’s hospitals of BJC HealthCare. WashU Medicine has a storied history in MD/PhD training, recently dedicated $100 million to scholarships and curriculum renewal for its medical students, and is home to top-notch training programs in every medical subspecialty as well as physical therapy, occupational therapy, and audiology and communications sciences.
Originally published on the WashU Medicine website