An atomic-level investigation of how Eastern equine encephalitis virus binds to a key receptor and gets inside of cells also has enabled the discovery of a decoy molecule that protects against the potentially deadly brain infection, in mice.
The study, from researchers at Washington University School of Medicine in St. Louis, is published Jan. 3 in the journal Cell. By advancing understanding of the complex molecular interactions between viral proteins and their receptors on animal cells, the findings lay a foundation for treatments and vaccines for viral infections.
“Understanding how viruses engage with the cells they infect is a critical part of preventing and treating viral disease,” said co-senior author Michael S. Diamond, MD, PhD, the Herbert S. Gasser Professor at Washington University. “Once you understand that, you have the foundation for developing vaccines and drugs to block it. In this study, it took us a long time to sort out the complexity associated with the particular receptor-virus interaction, but once we acquired this knowledge, we were able to design a decoy molecule that turned out to be very effective at neutralizing the virus and protecting mice from disease.”
Though infections of Eastern equine encephalitis virus in people are rare — with only a few cases reported worldwide each year — about one-third of those with the infection die, and many survivors suffer lasting neurological problems. Further, scientists predict that as the planet warms and climate change lengthens mosquito populations’ seasons and geographical reach, risk of infection will grow. At present, there are no approved vaccines against the virus or specific medications to treat it.
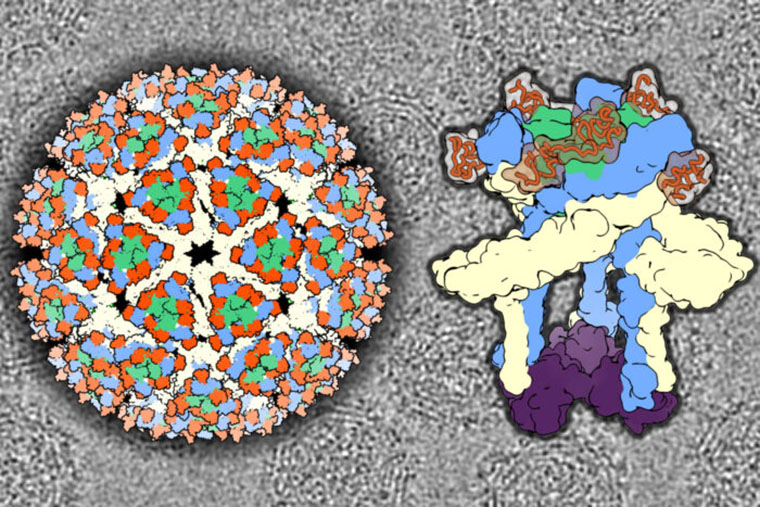
As a first step to finding ways to treat or prevent the deadly virus, Diamond and co-senior author Daved H. Fremont, PhD, a professor of pathology and immunology, set about investigating how the virus attaches to one of its key receptors — a molecule called VLDLR, or very-low density lipoprotein receptor. The molecule is found on the surface of cells in the brain and other parts of the body. Co-first author Lucas Adams, an MD/PhD student in the Fremont and Diamond laboratories, used cryo-electron microscopy to reconstruct the virus binding to the receptor in atomic-level detail.
The results turned out to be unexpectedly complex. The molecule is composed of eight repeated segments, called domains, strung together like beads on a chain. Usually, a viral protein and its receptor fit together in one very specific way. In this case, however, two or three different spots on the viral surface proteins were capable of attaching to any of five of the molecule’s eight domains.
“What’s really striking is that we find multiple binding sites, but the chemistry of each of the binding sites is very similar and also similar to the chemistry of binding sites for other viruses that interact with related receptors,” said Fremont, who is also a professor of biochemistry & molecular biophysics and of molecular microbiology. “The chemistry just works out well for the way viruses want to attach to cell membranes.”
The domains that make up this molecule also are found in several related cell-surface proteins. Similar domains are found in proteins from across the animal kingdom.
“Since they’re using a molecule that naturally has repetitive domains, some of the alphaviruses have evolved to use the same strategy of attachment with multiple different domains in the same receptor,” said Diamond, who is also a professor of medicine, of molecular microbiology, and of pathology and immunology. Alphaviruses include Eastern equine encephalitis virus and several other viruses that cause brain or joint disease. “There are sequence differences in the VLDLR receptor over evolution in different species, but since the virus has this flexibility in binding, it is able to infect a wide variety of species including mosquitoes, birds, rodents and humans.”
To block attachment, the researchers created a panel of decoy receptors by combining subsets of the eight domains. The idea was that the virus mistakenly would bind to the decoy instead of the receptor on cells, and the decoy with the virus attached could then be cleared away by immune cells.
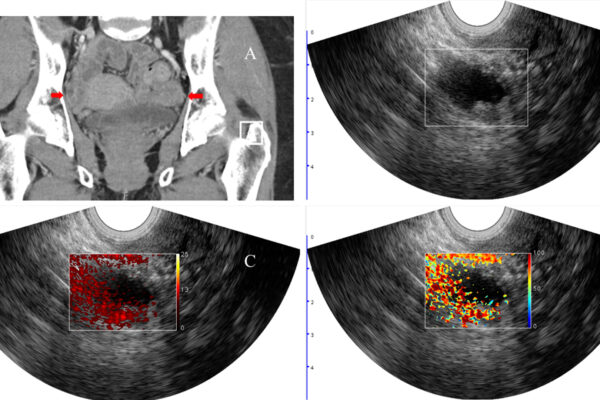
Co-first author Saravanan Raju, MD, PhD, a postdoctoral researcher in the Diamond lab, evaluated the panel of decoys. First, he tested them on cells in dishes. Many neutralized the virus. Then, he turned to mice. Raju pretreated mice with a decoy or saline solution, as a control, six hours before injecting the virus under their skin, a mode of infection that mimics natural infection via mosquito bite. Three decoys were tested: one known to be unable to neutralize the virus; one made from the full-length molecule; and one made from just the first two domains.
All of the mice that received saline solution, the non-neutralizing decoy or the full-length decoy died within eight days of infection. All of the mice that received the decoy made from the first two domains survived without signs of illness.
Certain aspects of its biology give Eastern equine encephalitis virus the potential to be weaponized, making it particularly important to find a way to protect against it. In a subsequent experiment in which the mice were infected by inhalation — as would happen if the virus were aerosolized and used as a bioweapon — the decoy made from the first two domains was still effective, reducing the mice’s chance of death by 70%.
“Through a combination of the structural work and the domain deletion work, we were able to figure out which domains are the most critical and create a quite effective decoy receptor that can neutralize viral infection,” Fremont said. “This study broadens what we know about virus-receptor interactions and could lead to new approaches to preventing viral infections.”
Adams LJ, Raju S, Ma H, Gilliland T, Reed DS, Klimstra WB, Fremont DH, Diamond MS. “Structural and functional basis of VLDLR usage by Eastern equine encephalitis virus.” Cell. Jan. 3, 2024. DOI: 10.1016/j.cell.2023.11.031
This research was supported by the National Institutes of Health (NIH), grant numbers R01 AI141436 and U19 AI142790 and contract number AI201800001; the National Institute of Allergy and Infectious Diseases, grant number R01AI095436 and contract number HHSN272201700060C; and the Defense Threat Reduction Agency, grant number MCDC2103-01. This content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Allergy and Infectious Diseases or the NIH.
Diamond is a consultant or adviser for Inbios, Ocugen, Vir Biotechnology, Topspin Therapeutics, Moderna, Merck, and Immunome. The Diamond laboratory has received funding support from Emergent BioSolutions, Moderna, and Vir Biotechnology. Fremont is a founder of Courier Therapeutics and has received funding support from Emergent BioSolutions and Mallinckrodt Pharmaceuticals.
About Washington University School of Medicine
WashU Medicine is a global leader in academic medicine, including biomedical research, patient care and educational programs with 2,800 faculty. Its National Institutes of Health (NIH) research funding portfolio is the third largest among U.S. medical schools, has grown 52% in the last six years, and, together with institutional investment, WashU Medicine commits well over $1 billion annually to basic and clinical research innovation and training. Its faculty practice is consistently within the top five in the country, with more than 1,800 faculty physicians practicing at 65 locations and who are also the medical staffs of Barnes-Jewish and St. Louis Children’s hospitals of BJC HealthCare. WashU Medicine has a storied history in MD/PhD training, recently dedicated $100 million to scholarships and curriculum renewal for its medical students, and is home to top-notch training programs in every medical subspecialty as well as physical therapy, occupational therapy, and audiology and communications sciences.
Originally published on the School of Medicine website