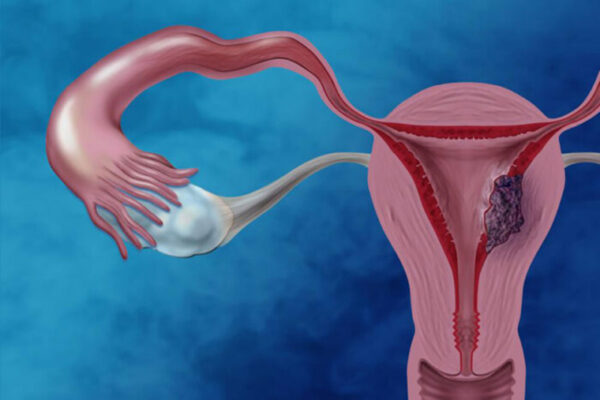
Cases of endometrial cancer — a gynecologic cancer of the lining of the uterus — have increased in recent decades, as have deaths caused by the condition. To spur new strategies to prevent and treat endometrial cancer, the National Cancer Institute (NCI) of the National Institutes of Health (NIH) has awarded researchers at Washington University School of Medicine in St. Louis a prestigious Specialized Programs of Research Excellence (SPORE) grant.
The five-year grant will provide about $11.6 million to research programs at Washington University, the University of New Mexico and the University of Oklahoma Health Sciences Center. The researchers dubbed the program the Route 66 Specialized Program of Research Excellence because of the three universities’ locations along historic Route 66, which crosses the Midwest and Southwest.
These locations provide an opportunity to better address endometrial cancer in patient populations that have been historically underrepresented in cancer research and clinical trials and are disproportionately affected by endometrial cancer, including Black, American Indian and Hispanic patients.
“Endometrial cancer is the most common gynecologic cancer and unfortunately — for reasons we don’t yet understand — is on the rise,” said principal investigator and gynecologic oncologist David G. Mutch, MD, the Ira C. and Judith Gall Professor of Obstetrics & Gynecology at Washington University. Mutch treats patients at Siteman Cancer Center at Barnes-Jewish Hospital and Washington University School of Medicine.
“We have been interested in this cancer for 30 years, but we have made very little headway in improving treatments or preventing it,” Mutch said. “As part of the new SPORE, we will be investigating three key areas for potential treatment and prevention strategies. We also hope our studies will be able to shed light on the racial disparities we see in this type of cancer.”
The funding will support three major research projects, each of which includes an early-phase clinical trial. One project team will investigate an inhibitor of important molecules called heat shock proteins. A second team will investigate inhibitors that target elements of more aggressive uterine cancer; these inhibitors block a key protein called the receptor tyrosine kinase AXL. And a third project will be focused on the possibility of early detection and prevention through weight-loss strategies.
The new grant also provides funding for resources supporting all of these research initiatives, including a biospecimen core; a biostatistics and bioinformatics core; a metabolomics core; an administrative core; and programs for innovative research and career development to recruit and mentor early-career investigators focused on understanding, treating and preventing endometrial cancer.
“This new SPORE grant will help our patients gain access to innovative clinical trials of treatment and prevention strategies that have the potential to improve clinical care for endometrial cancer,” said Dineo Khabele, MD, the Mitchell and Elaine Yanow Professor and head of the Department of Obstetrics & Gynecology at Washington University. “It will also help build a strong foundation of career support and training for early-career investigators, so they will be well positioned to continue this important work into the future.”
In one clinical trial focused on inhibiting heat shock protein, the researchers will investigate a drug called SHetA2. The investigational drug has been shown to interfere with the survival pathways of endometrial cancer cells. This project is led by Doris M. Benbrook, PhD, whose team developed the drug, and Kathleen N. Moore, MD, both of the University of Oklahoma.
A second clinical trial will investigate whether inhibiting a key protein called the receptor tyrosine kinase AXL will make the standard treatments for endometrial cancer, including the chemotherapy drug paclitaxel, more effective against aggressive tumors. This investigational drug, called AVB-500, is also known as batiraxcept. This project is led by Mutch; Matthew A. Powell, MD, a professor of obstetrics and gynecology at Washington University; and Katherine C. Fuh, MD, PhD, formerly of Washington University School of Medicine and now at the University of California, San Francisco.
In a third clinical trial, the researchers will focus on prevention. Since excess weight and obesity are associated with endometrial cancer, the researchers will investigate whether weight loss can prevent the development of endometrial cancer in women with endometrial hyperplasia, a precancerous condition in which the uterine lining becomes too thick. The researchers will investigate whether the addition of weight-loss interventions combined with progestin treatment for hyperplasia helps women avoid hysterectomy when fertility preservation is a goal. The translational research will focus on how helpful changes in metabolism can lead to long-term health and ability to achieve pregnancy. This project is led by Andrea R. Hagemann, MD, an associate professor of obstetrics and gynecology at Washington University; and Kimberly K. Leslie, MD, of the University of New Mexico.
“We are excited to be able to provide our patients with opportunities to participate in clinical trials of innovative therapies and prevention strategies that have solid science behind their designs,” Mutch said. “We also are hopeful these trials will give patients who historically have not had opportunities to participate in research the option to do so. And with that, we hope to develop a better understanding of racial disparities in endometrial cancer, so we can take steps to reduce them.”
This work is supported by the NCI of the NIH, grant number 1P50CA265793-01A1.
About Washington University School of Medicine
WashU Medicine is a global leader in academic medicine, including biomedical research, patient care and educational programs with 2,800 faculty. Its National Institutes of Health (NIH) research funding portfolio is the third largest among U.S. medical schools, has grown 52% in the last six years, and, together with institutional investment, WashU Medicine commits well over $1 billion annually to basic and clinical research innovation and training. Its faculty practice is consistently within the top five in the country, with more than 1,800 faculty physicians practicing at 65 locations and who are also the medical staffs of Barnes-Jewish and St. Louis Children’s hospitals of BJC HealthCare. WashU Medicine has a storied history in MD/PhD training, recently dedicated $100 million to scholarships and curriculum renewal for its medical students, and is home to top-notch training programs in every medical subspecialty as well as physical therapy, occupational therapy, and audiology and communications sciences.