Between natural infection and a global vaccination campaign, most people now have some immunity against the virus that causes COVID-19. This widespread immunity hasn’t stopped people from getting infected, but it has dampened the massive waves of illness and death that roiled the globe in the early years of the pandemic. Keeping the virus in check requires maintaining this level of immunity, a difficult task because the virus is constantly spinning off new variants that can partially evade antibodies elicited by vaccines and prior infections.
New research from scientists at Washington University School of Medicine in St. Louis suggests that updated booster shots will be important for shoring up population immunity as new variants emerge — but there’s a caveat.
Their research, published April 3 in Nature, shows that vaccinating people against the original strain of the virus and then boosting with a shot that targets a new variant can elicit a broad antibody response capable of neutralizing a wide array of variants, including ones that have not yet emerged. The trick is to target a variant for the booster that is so different from the original strain of the virus that it triggers the maturation of new and diverse antibody-producing cells.
“The challenge with COVID-19 is that the virus keeps mutating,” said senior author Ali Ellebedy, an associate professor of pathology and immunology, of medicine, and of molecular microbiology. “It’s not that the vaccines don’t elicit a lasting antibody response. They do. The problem is that the virus changes and the existing antibodies become irrelevant. Here we showed that it’s possible to design a variant-specific booster that doesn’t just strengthen the antibodies people already have but elicits new antibodies. This means that periodically giving boosters targeting new variants would allow population-level protection to be maintained even as the virus evolves.”
The first COVID-19 vaccines reduced the risk of severe illness and death by more than 90%. But then the virus changed. The antibodies that had worked so well against the original strain proved less effective at recognizing and neutralizing emerging variants, leading to breakthrough infections. The obvious solution was to update the vaccines to target new variants, but the success of the first vaccines against the original strain made designing an effective variant booster shot tricky, Ellebedy said.
“The whole point of making boosters against new variants is to teach the immune system to recognize features in the new variants that are different from the original strain,” Ellebedy said. “But the new variants still share a lot of features with the original strain, and it’s possible that the response to these shared features could dominate the response to new features. The boosters could end up just engaging immune memory cells that are already present rather than creating new memory cells, which is what we need for protection against new variants.”
To gauge the effectiveness of boosters at eliciting new antibodies, Ellebedy and colleagues studied people who received a COVID-19 vaccine targeted against the original strain, followed by a combined booster targeting two of the early variants — beta and delta — or a booster targeting the newer omicron variant. Along with Ellebedy, the research team included co-corresponding author Jackson Turner, an instructor in pathology and immunology, and co-first authors Wafaa B. Alsoussi, a graduate student, and Sameer Kumar Malladi, a postdoctoral researcher, both in Ellebedy’s lab.
The first studies were discouraging, Ellebedy noted. The researchers looked at 39 people who had received the two-shot primary sequence of the Pfizer/BioNTech or Moderna COVID-19 vaccines, followed by an experimental booster shot targeting the beta and delta variants. All participants produced antibodies that neutralized the original virus strain and the beta and delta variants. But none of the antibodies studied were unique to beta or delta. The absence of such antibodies indicates that the variant booster had failed to trigger the development of detectable new antibody-producing cells, Ellebedy said.
“This was disappointing but not surprising,” said Ellebedy, who is also an expert on influenza vaccines. “If you look at the sequences for the beta and delta spike proteins, they are not really very different from the original strain. If we saw this degree of difference among influenza strains, we would say there’s no reason to update the annual vaccine. But the omicron variant is a different matter.”
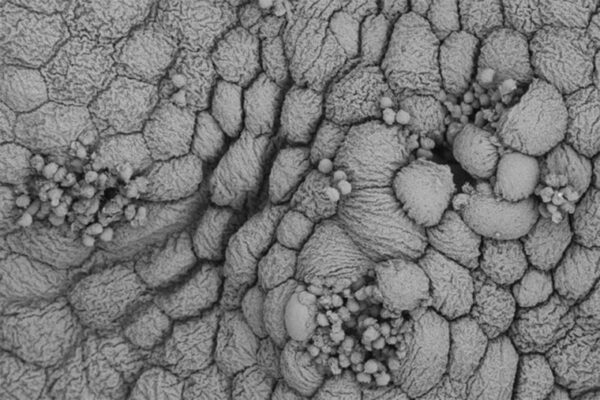
The omicron variant, dominant worldwide since late 2021, carries dozens of new mutations relative to the original strain of the virus. Ellebedy and colleagues recruited eight people who had received the Pfizer/BioNTech or Moderna COVID-19 vaccine and gave them a booster targeted against the omicron variant alone. The CDC later recommended the use of updated boosters that target both the omicron variant and the original strain. Such bivalent boosters became available to the public in fall 2022, manufactured by both Pfizer/BioNTech and Moderna.
Studying blood samples provided by participants four months after their boosters, the researchers identified more than 300 distinct antibodies capable of neutralizing the original strain, or one or more of the variants. Of those, six neutralized omicron but not the original strain, an indication that the booster successfully triggered the creation of new antibodies optimized for omicron. One such new antibody even neutralized BA.5, a subvariant of omicron that is circulating widely now but had not yet emerged at the time the booster was made.
“This booster engaged naive B cells and created new memory cells, which means it expanded people’s immune repertoire and equipped them to respond to a greater diversity of variants,” Ellebedy said. “Designing boosters to maintain immunity to the evolving virus is not going to be easy. The extent of the difference between the old and the new variants is clearly important. But if we are careful about how we choose which variants to include in boosters, I think we can stay ahead of this virus.”
Alsoussi WB, Malladi SK, Zhou JQ, Liu Z, Ying B, Kim W, Schmitz AJ, Lei T, Horvath SC, Sturtz AJ, McIntire KM, Evavold B, Han F, Scheaffer SM, Fox IF, Mirza S, Parra-Rodriguez L, Nachbagauer R, Nestorova B, Chalkias S, Farnsworth CW, Klebert MK, Pusic I, Strnad BS, Middleton WD, Teefey SA, Whelan SPJ, Diamond MS, Paris R, O’Halloran JA, Presti RM, Turner JS, Ellebedy AH. SARS-CoV-2 Omicron boosting induces de novo B cell response in humans. Nature. April 3, 2023. DOI: 10.1038/s41586-019-0000-0
This work was supported by the National Institutes of Health (NIH), grant numbers U01AI141990, 1U01AI150747, 5U01AI144616-02, R01AI168178-01, R01 AI157155 and R01 AI163019; and by Moderna Inc.
About Washington University School of Medicine
WashU Medicine is a global leader in academic medicine, including biomedical research, patient care and educational programs with 2,800 faculty. Its National Institutes of Health (NIH) research funding portfolio is the third largest among U.S. medical schools, has grown 52% in the last six years, and, together with institutional investment, WashU Medicine commits well over $1 billion annually to basic and clinical research innovation and training. Its faculty practice is consistently within the top five in the country, with more than 1,800 faculty physicians practicing at 65 locations and who are also the medical staffs of Barnes-Jewish and St. Louis Children’s hospitals of BJC HealthCare. WashU Medicine has a storied history in MD/PhD training, recently dedicated $100 million to scholarships and curriculum renewal for its medical students, and is home to top-notch training programs in every medical subspecialty as well as physical therapy, occupational therapy, and audiology and communications sciences.