The immune system is the brain’s best frenemy. It protects the brain from infection and helps injured tissues heal, but it also causes autoimmune diseases and creates inflammation that drives neurodegeneration.
Two new studies in mice suggest that the double-edged nature of the relationship between the immune system and the brain may come down to the origins of the immune cells that patrol the meninges, the tissues that surround the brain and spinal cord. In complementary studies published June 3 in the journal Science, two teams of researchers at Washington University School of Medicine in St. Louis unexpectedly found that many of the immune cells in the meninges come from bone marrow in the skull and migrate to the brain through special channels without passing through the blood.
These skull-derived immune cells are peacekeepers, dedicated to maintaining a healthy status quo. It’s the other immune cells, the ones that arrive from the bloodstream, that seem to be the troublemakers. They carry genetic signatures that mark them as likely to promote autoimmunity and inflammation, and they become more abundant with aging or under conditions of disease or injury. Taken together, the findings reveal a key aspect of the connection between the brain and the immune system that could inform our understanding of a wide range of brain disorders.
“There has been this gap in our knowledge that applies to almost every neurological disease: neuro-COVID, Alzheimer’s disease, multiple sclerosis, brain injury, you name it,” said Jonathan Kipnis, PhD, the Alan A. and Edith L. Wolff Distinguished Professor of Pathology & Immunology and a BJC Investigator. Kipnis is the senior author on one of the papers. “We knew immune cells were involved in neurological conditions, but where were they coming from? What we’ve found is that there’s a new source that hasn’t been described before for these cells.”
Earlier this year, Kipnis showed that immune cells stationed in the meninges keep tabs on the brain. As part of these new studies, Kipnis and Marco Colonna, MD, the Robert Rock Belliveau, MD, Professor of Pathology and the senior author on the other paper, independently launched projects to find where such cells come from. Kipnis focused on the innate arm of the immune system and Colonna on the adaptive arm. Innate immune cells are responsible for inflammation, which helps defend against infection and heal injuries, but also can damage tissues and contribute to degenerative conditions such as Alzheimer’s and Parkinson’s disease. Adaptive immune cells are capable of specifically targeting undesirables such as viruses and tumors, but they also can mistakenly home in on the body’s own healthy tissues, resulting in autoimmune diseases such as multiple sclerosis.
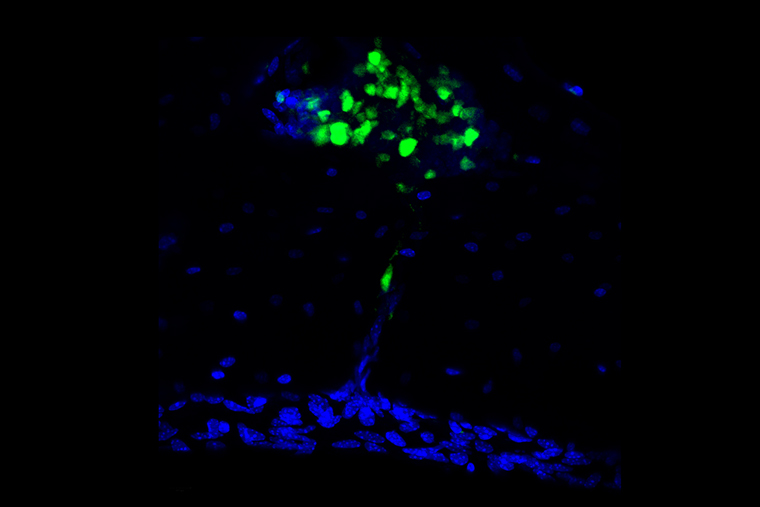
Colonna and colleagues — including co-first authors Simone Brioschi, PhD, a postdoctoral researcher, Wei-Le Wang, PhD, a postdoctoral researcher, and Vincent Peng, a graduate student — traced the development of B cells, antibody-producing members of the adaptive immune system. They found that most B cells in the meninges arose and matured in the skull bone marrow. As B cells mature, they must be taught to distinguish between normal proteins from the body, which pose no threat, and foreign proteins that signal infection or disease and require a response. For B cells destined for a life patrolling the boundaries of the central nervous system, the skull is a convenient site for this education.
“B cells in the bone marrow of the skull come into contact with the central nervous system and are educated by the central nervous system,” said Colonna, who is also a professor of medicine. “That would not happen if they were released into the blood. Because they are directly in contact with the brain, they learn to be tolerant of brain proteins.”
Along with the tolerant B cells derived from the skull, the researchers also discovered a population of B cells that come into the meninges from the blood. These blood-derived B cells are not trained to ignore normal central nervous system proteins. Some of these cells may wrongly recognize harmless central nervous system proteins as foreign and produce antibodies against them, Colonna said. Moreover, the number of these blood-derived B cells increases with age, providing a clue to why the risk of neuro-immune conditions is higher in older people.
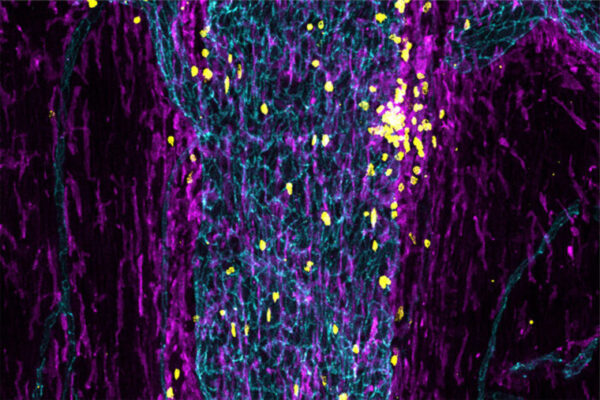
Meanwhile, Kipnis’ team — led by co-first authors Andrea Cugurra, a graduate student, Tornike Mamuladze, MD, a visiting researcher, and Justin Rustenhoven, PhD, a postdoctoral researcher — was searching for the source of meningeal myeloid cells, a group of innate immune cells. They found that myeloid cells arose in the bone marrow of the skull and spinal vertebrae and entered the meninges via direct channels through the bone.
Using mouse models of multiple sclerosis and of brain and spinal cord injuries, Kipnis and colleagues found that myeloid cells swarm into the brain and spinal cord in response to injury or disease. Most of the entering cells are drawn from the resident population of myeloid cells in the meninges. These are biased toward regulating and modulating the immune response. But some myeloid cells come in from the blood, and these are more inflammatory, capable of causing damage if not properly controlled.
“Understanding where these cells come from and how they behave is a critical part of understanding the basic mechanisms of neuro-immune interactions, so we can design new therapeutic approaches for neurological conditions associated with inflammation,” said Kipnis, who is also a professor of neurosurgery, of neurology and of neuroscience. “The location of these cells in the skull makes them relatively accessible, and opens up the possibility of designing therapies to alter the behavior of these cells and treat neuro-immune conditions.”
Cugurra A, Mamuladze T, Rustenhoven J, Dykstra T, Beroshvili G, Greenberg ZJ, Baker W, Papadopoulos Z, Drieu A, Blackburn S, Kanamori M, Brioschi S, Herz J, Schuettpelz LJ, Colonna M, Smirnov I, Kipnis J. Skull and vertebral bone marrow are myeloid cell reservoirs for the meninges and CNS parenchyma. Science. June 3, 2021.
The study on myeloid cells was supported by the National Institutes of Health, grant numbers AT010416, AG034113 and AG057496.
Brioschi S, Wang W-L, Peng V, Wang M, Shchukina I, Greenberg ZJ, Bando JK, Jaeger N, Czepielewski RS, Swain A, Mogilenko D, Beatty WL, Bayguinov P, Fitzpatrick JAJ, Schuettpelz LG, Fronick CC, Smirnov I, Kipnis J, Shapiro VS, Wu GF, Gilfillan S, Cella M, Artyomov MN, Kleinstein SH, Colonna M. Heterogeneity of meningeal B cells reveals a lymphopoietic niche at the CNS borders. Science. June 3, 2021.
The study on B cells was supported by the National Institutes of Health (NIH), grant numbers R01AI104739, F30 DK127540-01 and T32 DK 77653-28; the Gruber Foundation; and the Lawrence C. Pakula, MD, IBD Education & Innovation Fund, fellowship number FA-2020-01-IBD-1.1.
Washington University School of Medicine’s 1,500 faculty physicians also are the medical staff of Barnes-Jewish and St. Louis Children’s hospitals. The School of Medicine is a leader in medical research, teaching and patient care, consistently ranking among the top medical schools in the nation by U.S. News & World Report. Through its affiliations with Barnes-Jewish and St. Louis Children’s hospitals, the School of Medicine is linked to BJC HealthCare.