For the past year, Deniz Ercan-Fang, a senior in Arts & Sciences at Washington University in St. Louis, has spent his Saturdays interviewing veterans receiving palliative or hospice care, simply asking them their story.
“One of the veterans that I worked with had problems with breathing, so we couldn’t do much of a story at a time,” Ercan-Fang said. “We would do five- to 10-minute segments at a time, usually once or twice a day. Over a few weeks, I really got to know this veteran. When he read what I wrote about his mother, he started to cry and stopped reading the story. He gave me a hug right in the middle of it because he thought that the way that I captured his mother was the way that he would have done it. It was very touching.”
Ercan-Fang is a pre-med senior who is majoring in anthropology and biochemistry, with a minor in biology, all in Arts & Sciences. He is one of three students in the inaugural class of local volunteers for a program called “My Life, My Story.” Five additional students joined the effort this fall.

The St. Louis Veterans Affairs (VA) Medical Center – Jefferson Barracks is one of a handful of VA facilities across the nation participating in “My Life, My Story.” Patients in the hospice and palliative care section of the hospital are offered the opportunity to have a version of their life story added to their official medical files. Trained volunteers from Washington University’s Medicine & Society Program (MedSoc) in Arts & Sciences conduct the interviews that form the core of these stories.
The student volunteers write 1,000-word, first-person accounts about the experiences each veteran shared. The story is then read to the veteran, edited again and finally incorporated into the veteran’s official medical file so that nurses and doctors can better understand their patients.
“Writing down the life story really helps us to meet the patients where they are,” said Poonam Jain, MD, medical director of hospice and palliative care at Jefferson Barracks. “It helps us to know what the patient wants and needs moving forward.”
Jain worked hard to bring “My Life, My Story” to St. Louis after she heard about the program created and run by Thor Ringler at the William S. Middleton Memorial Veterans Hospital in Madison, Wis. The effort is part of a larger Whole Health initiative, a transformational health-care model adopted by the Veterans Health Administration as part of its mission to support the health and well-being of veterans.
“‘My Life, My Story’ is part of a cultural shift in the way we do health care here,” said Jason Horn, a Whole Health coach at Jefferson Barracks, who helps train the student volunteers. “Whole Health focuses on the veteran — what they want for their care and what matters most for them.”
Finding an authentic voice
Washington University is the only school in the St. Louis area working with the VA to provide this program.
Anna Jacobsen, lecturer in anthropology in Arts & Sciences, is assistant director of Washington University’s MedSoc program and its administrator. “I am looking for students with the willingness to commit the time and compassion for stories that may not resemble anything they’ve experienced in their lives,” she said.
Students like Aaron Bao, a pre-med junior majoring in biology and Chinese with a minor in anthropology, all in Arts & Sciences. Bao and Ercan-Fang completed training to prepare in the weeks prior to their first interviews. In Jacobsen’s course, “Health and Wellness in the Community: A Service Learning Seminar,” which is required for all MedSoc students, she includes medical privacy law training and ethnographic interview practice.

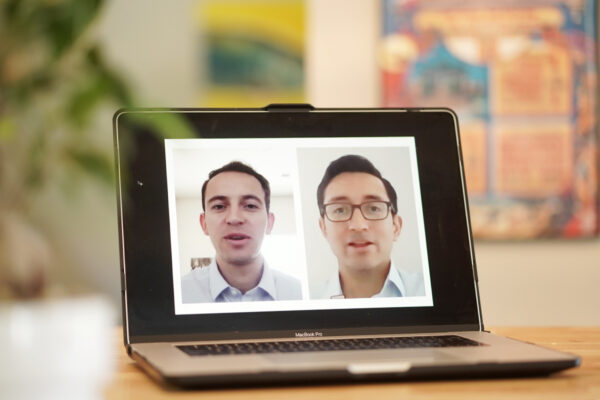
Before interviewing the veterans for the first time, Bao and Ercan-Fang were nervous about relating to their stories and successfully writing in the veteran’s voice. But, after some practice, they realized that their stories transcend time and personal experience.
“I was a little worried about making sure that their voice sounded like themselves,” Ercan-Fang said. “But, I think that following the transcripts and realizing I didn’t have to edit their transcripts helped. I realized those are their words, and I got more confident in what I wrote.”
“I think the fact that their stories are in first person motivates you to keep it genuine and authentic,” Bao said. “When you talk to them, you realize that a lot of them are interested in things that you wouldn’t have expected them to be interested in. So they feel a lot of times less like interviews and more like just conversations.”
Seeing humanity in a different way
The guidelines for the interviews encourage the veterans to speak about people or experiences about which they feel passionate.
“The main point is that these are the patients’ stories. They can really talk about whatever they want to talk about,” Ercan-Fang said. “I’ve had many veterans that suffer from some form of PTSD, and they don’t want to talk about their service. So instead, we focus on their family afterwards, early childhood, their parents, their siblings, or anything else they want to talk about.”

Jacobsen acknowledges that these experiences provide lifelong lessons to the students. Students are able to “see humanity in a different way,” she said.
“The students’ responses are great, humbling, profound and sometimes frustrated,” Jacobsen said. Many of the veterans have had fulfilling lives, and they prefer to talk about their families, their jobs and their hobbies instead of their military experiences. Other interviews are emotional and confront difficult realities. “I think that’s important to understand that life and time may not always be fair, it doesn’t work the same way for everyone,” she said.
Bao said every interview he conducts is inspiring. “One veteran said that after his service he couldn’t find a job,” he said. “He was homeless for about 20 years, addicted to drugs, and lost touch with his entire family. But now, I really couldn’t tell that he had been through such a hardship because he was funny and charming.
“I asked him, ‘Where did you kind of find the motivation to pull yourself out from a hole like that?’ And he just told me that one day he woke up and wanted to get better.”
Humanizing patients
The larger goal of “My Life, My Story” is to personalize the doctor-patient relationship and to bring narrative practices to all medical fields. The project team believes that each veteran has a life story worth telling.
“People want to be seen as people, and I think this is what these students are doing,” Jacobsen said.
The veterans, too, find the experience meaningful. Not only do they receive more personalized care from their doctors and nurses, but also, for some, the interview is the first time they’ve had their voice put down on record. It can be therapeutic for the veterans to share their life experiences with not only their medical professionals, but their family as well.
“At the St. Louis VA, some of the vets get multiple copies to hand out to their families,” Jacobsen said. “These stories have been read at reunions, funerals.”
Bao and Ercan-Fang, both aspiring physicians, want to use what they have learned in these interviews in their own medical careers. They hope to encourage doctors and nurses to treat their patients holistically by using narrative medicine.
“It’s looking at diseases from very encompassing point of view,” Bao said. “It considers the experiences, the patient’s environment, the way the patient was raised, your outlook on the world, and the structural forces that surround the patient.”
“I think it’s about understanding that the numbers are not just patients with a specific disease, but rather a person with an identity and a history,” Ercan-Fang said.