As people age, it can be hard to predict whether they will develop Alzheimer’s disease. With the exception of a few people with strong family histories of the disease, doctors don’t know who will develop Alzheimer’s, at what age or how quickly it will progress.
Two new studies led by Washington University School of Medicine in St. Louis aim to clarify the genetic underpinnings of Alzheimer’s, a disease characterized by memory loss and cognitive decline. By studying the DNA of thousands of people, the researchers seek to identify genetic factors that raise or lower the risk of developing the disease. They also intend to find and characterize markers of the disease in the cerebrospinal fluid that surrounds the brain and spinal cord and identify new treatments.
The studies are funded by two grants totaling $7 million from the National Institute on Aging of the National Institutes of Health (NIH) and led by Carlos Cruchaga, an associate professor of psychiatry and of neurology at the School of Medicine.

“We are taking two different approaches with the same goal: to understand the genetic architecture of Alzheimer’s disease so we can figure out why some people develop the disease and others don’t,” Cruchaga said. “Both approaches are unbiased — meaning we are going in with no expectations about what genetic variants or genes we are going to find.”
One set of studies is population-based. Cruchaga and colleagues will scan the genomes of about 4,000 people, some of whom have Alzheimer’s and others who don’t. They will compare the people’s genetic variations with known molecular signs of Alzheimer’s disease. Such molecular signs, also known as biomarkers, include levels of the protein tau and the protein fragment amyloid beta in the cerebrospinal fluid. The brains of Alzheimer’s patients are characteristically spotted with tau tangles and amyloid beta plaques.
The other set of studies looks at families with more than one member diagnosed with Alzheimer’s disease. Such families likely carry genetic risk factors for the disease. Researchers will study DNA from 1,260 people from 345 families, comparing individuals who developed Alzheimer’s with their relatives who did not, to look for genes associated with an elevated risk or, especially, a reduced risk of Alzheimer’s. Few genes are known that reduce risk, but they could be crucial for understanding why some people do not develop the disease.
An example is the Apolipoprotein E (ApoE) protein, which is involved in regulating levels of amyloid beta in the brain. The variant known as APOE4 raises the risk of developing Alzheimer’s disease threefold to fifteenfold, making it the largest known genetic risk factor for late-onset Alzheimer’s disease. The variant known as APOE2, on the other hand, reduces the risk of developing Alzheimer’s disease by 40 percent.
The researchers are particularly interested in elderly people who carry ApoE4 but who have not developed Alzheimer’s disease. Such people are likely to carry other genes that neutralize the high risk of ApoE4.
“Finding a resilience gene tells us that it plays an important role in the biology of Alzheimer’s disease,” Cruchaga said. “It tells us that differences in that specific gene or pathway can affect outcomes.”
Once genetic variants associated with Alzheimer’s disease are identified, the researchers will study whether genetic information can be combined with molecular and cellular markers of the disease to improve diagnosis and predictions of the disease.
Ideally, biomarkers would predict not only whether someone will develop Alzheimer’s, but at what age and how quickly the disease will progress. To that end, Cruchaga and colleagues will analyze a database they developed that includes information from nearly 4,000 Alzheimer’s patients, including genetic data, measures of the cerebrospinal fluid levels of Alzheimer’s-associated proteins, and results of tests of cognitive function, such as memory, taken repeatedly over years. The goal is to find genetic and molecular markers that predict the age at which people will develop Alzheimer’s symptoms and how quickly they will decline.
Several such biomarkers have been developed, but they are limited to research studies and are not used in clinical practice.
“I think the biomarker part is almost there,” Cruchaga said. “One of the reasons that biomarkers aren’t used in the clinic is that if we identify people with preclinical Alzheimer’s, we can’t actually do anything for them. What we need now is an intervention.”
There currently is no proven way to prevent or stop the cognitive decline of Alzheimer’s disease, let alone reverse it. Most of the drugs that have been or are being tested target amyloid beta. These studies may identify new therapeutic targets.
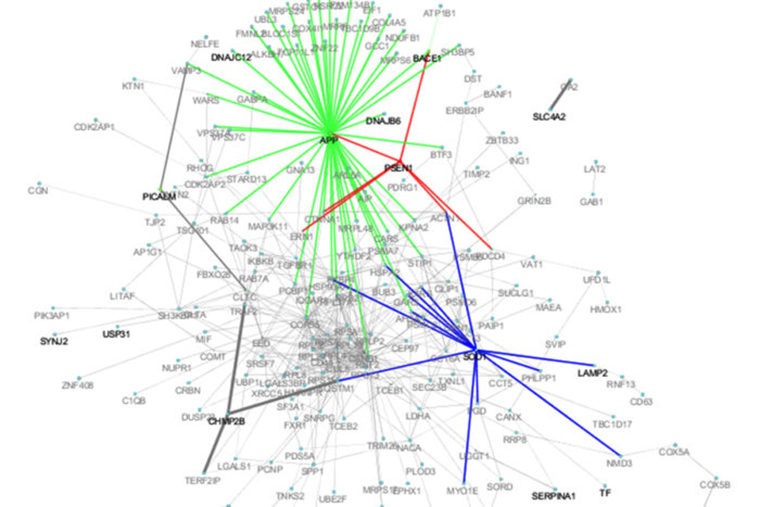
Every gene is part of one or more biological pathways, such as the lipid metabolism pathway or the debris clearance pathway. Pathways can involve dozens of genes, some of which turn up and others turn down the activity of the pathway.
Any spot on the pathway potentially could be targeted, not just the specific gene implicated in Alzheimer’s disease. By considering the whole pathway, the number of potential drug targets increases enormously. Cruchaga believes there may be drugs already available that target elements of the pathway.
“Scientists have known for a while that the amyloid beta pathway is important,” Cruchaga said. “What we’re trying to do is find out which other pathways are important, so we can start figuring out how we can make changes to those pathways.”
The long-term goal is to identify people at risk of developing Alzheimer’s many years in advance and then treat them so they never get the disease.
“Think about heart disease,” Cruchaga said. “You go to the doctor and they do a blood test and find that you have high cholesterol, high lipid levels. Your doctor tells you that you are at risk of a heart attack and prescribes you drugs so, hopefully, you never have a heart attack. This would be similar. Doctors could take a sample of your biomarkers, or perhaps image your brain, and if you are at risk based on those screening tests, then they could prescribe you drugs, with the goal that you never develop Alzheimer’s disease.”
Such a treatment regimen would be many years in the future, after any potential drugs are tested in cells, animals and people.