When the first antibiotics became available 70 years ago, they were often described as miracles of human ingenuity, rather like plastics or bright permanent dyes, which were discovered at roughly the same time. Packaged in vials or pills, they seemed like our inventions rather a chance gift of evolution and one that evolution might also rescind.
And so it proved. At first bacterial populations expressed only low levels of resistance to antibiotics. But soon, microbes were showing resistance to every new antibiotic within a few years of its introduction. Today, as scientists look for replacements for our dwindling stock of antibiotics, evolution is never far from their minds.
Given the failure of the pipeline for conventional antibiotics, scientists have been looking at the bacteria-killing potential of other classes of compounds. Typically, these are billed, at least initially, as less likely to trigger resistance.
But are they really?
One group of compounds again in the news is the bacteriocins, potent antimicrobial peptides (bits of proteins) that bacteria secrete that kill closely related bacteria. They were the subject of R. Fredrik Inglis’ doctoral research in the lab of Angus Buckling at the University of Oxford in the United Kingdom.
“When people again started proposing bacteriocins as novel therapeutics, we wondered if they could evolve resistance,” said Inglis, who is now a research scientist at Washington University in St. Louis.
To find out, he and his colleagues ran an “evolution experiment,” growing a strain of bacteria sensitive to a bacteriocin in the presence of a strain that produces the bacteriocin but is itself immune to it. By repeatedly transferring bacteria to fresh growth media, they were able to follow the bacteria for about 70 generations.
Their results, published Feb. 26 in the online edition of ISME Journal, the journal of the International Society Microbial Ecology, showed this bacteriocin isn’t resistance proof, but that strains that became resistant to it also became weaker, Inglis said.
Inglis attributes this success to the fact that the bacteriocin targets a receptor on the bacteria’s cell surface that is essential to its survival. This reduces the chance of resistance evolving — or at least makes resistance extremely costly in many natural environments.
Because they are specific to particular strains of bacteria, bacteriocins will not replace general antibiotics, but they could be used to target strains of multidrug resistant or highly virulent bacteria.
Would you like a little iron with that?
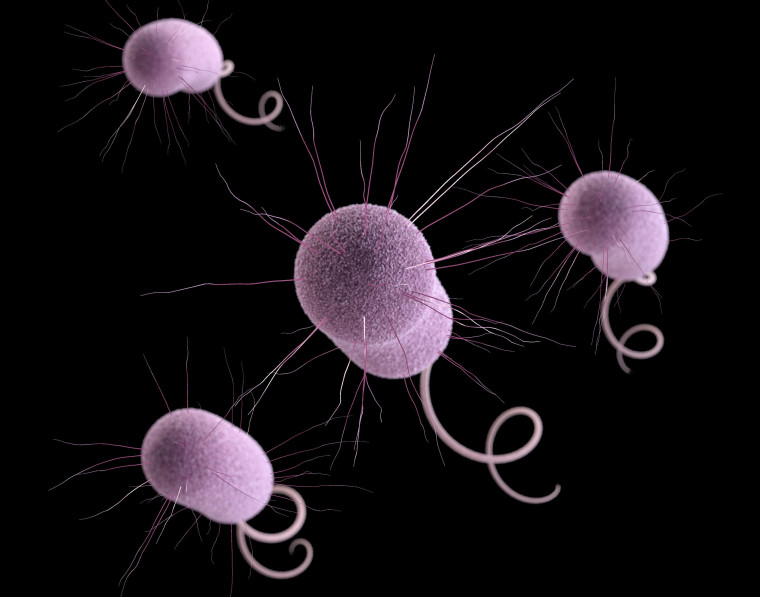
The bacterium was Pseudomonas aeruginosa, a prototypical multidrug resistant pathogen that serves as a model organism in the Buckling lab. Once limited to burn wounds, P. aeruginosa now causes severe hospital-acquired infections and persistent lung infections in cystic fibrosis patients.
Most P. aeruginosa produce bacteriocins called pyocins, typically several of them. The strain in this experiment produced three, two of which have rod-like structures and a third, called an S-type pyocin that is soluble and disappears in liquids.
The scientists knew that the S-type pyocin, which kills by degrading DNA, had to enter bacteria to kill them. They also knew that it entered bacteria by sneaking through siderophore receptors.
 Siderophore receptors are the bacterial equivalent of Achilles’ heel. Like all living organisms bacteria need iron, an element that easily swaps electrons, to conduct the business of life. Iron is one of the most abundant elements on the planet, but very little of it is in a soluble form bacteria and other living things can use.
Siderophore receptors are the bacterial equivalent of Achilles’ heel. Like all living organisms bacteria need iron, an element that easily swaps electrons, to conduct the business of life. Iron is one of the most abundant elements on the planet, but very little of it is in a soluble form bacteria and other living things can use.
This is particularly true within the human body, where iron is concealed in cells and large iron-binding proteins as a first line of defense against infection. So to garner enough iron to survive, bacteria secrete small molecules called siderophores to seek out iron in the environment and bring it back into the cell through siderophore-specific receptors.
Since bacteria make more of these receptors under iron-poor conditions, Inglis and his colleagues ran two sets of experiments: one in iron-rich media, and the other in iron-poor media.
When iron was freely available, the bacteria didn’t need to make the siderophore receptors and resistance to the pyocin evolved easily and often. “We had replicate evolving populations and the majority of them evolved resistance,” Inglis said.
When iron was limiting, the bacteria had to express the receptors to survive. Resistance to pyocin didn’t evolve very often and, when it did, the resistant bacteria grew very slowly. So resistance was costly in the iron-poor environment.
To test resistant bacteria farther, the scientists took bacteria that had evolved resistance under iron-rich conditions and transferred them to iron-poor ones. Even though resistance evolved easily in iron-rich conditions, which suggested that the resistant bacteria weren’t at a competitive disadvantage, when the resistant bacteria were under iron limitation, they grew poorly.
Why might this be important? In the iron-poor environment of the human body, where the iron concentration is about one atom per 1.6 liters of blood, initially susceptible P. aeruginosa might find it difficult to develop resistance to pyocin and resistant P. aeruginosa might grow so slowly the immune system would be able to clear them, Inglis said.
Taking bacteria seriously
The pyocin-resistance experiment is part of a larger reconsideration of bacteria not just as threat to our health but also as organisms in their own right, with their own ecology and evolutionary histories.
In retrospect, it is somewhat bizarre that nobody in the golden era of antibiotics questioned why soil bacteria make medicines for human illnesses.
The usual explanation was that soil bacteria are fiercely competitive, continually fighting for living space in the soil under our feet and that antibiotics are a happy side-effect of this ongoing microbial battle.
Chastened by the rise of resistance, scientists aren’t sure this basic assumption is entirely true, in part because the concentrations of antibiotic compounds in natural environments are so low as to be undetectable.
Some have proposed that antibiotics are inter-cellular signaling molecules and that both producing and receiving organisms may have developed enzymes that inactivated the antibiotics (resistance) in order to turn off the signal.
Others, including Washington University’s Gautam Dantas, assistant professor of pathology and immunology in the School of Medicine, have suggested that antibiotics might serve soil bacteria as sources of carbon and nitrogen; in this case inactivation (resistance) is really just digestion.
Inglis himself has made an intriguing suggestion. Perhaps bacteriocins, if not antibiotics, exist not to help bacteria but rather to ensure their own survival. In an experiment published in 2013, Inglis and colleagues showed that bacteriocins can act primarily as selfish genetic elements promoting their own transmission in the population.
Antibiotic resistance looks very different from a bacterial point of view than from our own.