Compared with routine medical care, probiotics administered to critically ill patients in intensive care units showed no benefit in preventing the colonization of drug-resistant microbes in the intestinal tract, according to new research at Washington University School of Medicine in St. Louis.
Probiotics — live microorganisms believed to help
restore the balance of intestinal bacteria and increase resistance to
harmful germs — were given to patients twice daily for up to two weeks.
But they were no more effective than not giving probiotics, the
researchers report Aug. 27 in Infection Control & Hospital Epidemiology.
“Probiotic use is an intriguing topic,” said Jennie H. Kwon, DO, lead author of the study and a clinical researcher in the Division of Infectious Diseases. “With fewer therapies available to treat multidrug-resistant organisms, innovative methods to prevent or eliminate gastrointestinal colonization are necessary.”
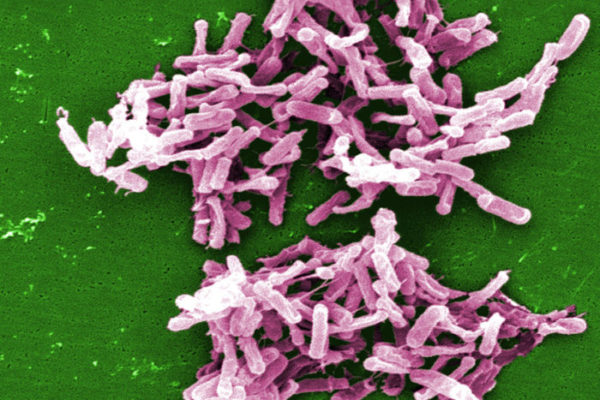
Drug-resistant “superbugs” pose a serious risk to hospitalized patients —particularly those in ICUs — because the microbes increase the risk of hard-to-treat infections that can spread easily.
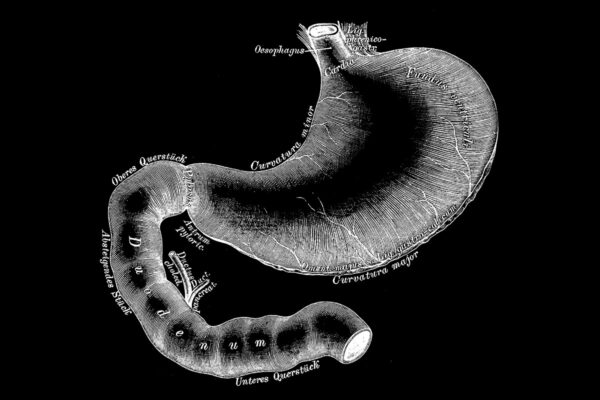
The pilot study followed 70 patients admitted to ICUs at Barnes-Jewish Hospital in St. Louis. Researchers studied whether the probiotic Lactobacillus rhamnosus GG could prevent the intestinal colonization of superbugs such as Clostridium difficile (C. diff), vancomycin-resistant Enterococcus (VRE) and Pseudomonas aeruginosa.
Patients were randomly assigned to receive probiotics and routine care or routine care alone. The researchers then monitored whether the microbes took up residence in the intestinal tract — a first step to developing a full-blown infection.
The data showed that the drug-resistant microbes colonized the intestinal tracts of 10 percent of patients in the probiotic group and 15 percent in the standard-care group — a difference that was not statistically significant.
However, Kwon emphasized the study’s limitations: small patient sample size, brief length of patient follow-up, and use of a single type and dose of probiotic. Additionally, the researchers confined the study to gastrointestinal bacteria and did not assess the possible impact of probiotics on preventing the colonization of superbugs in the stomach or the upper airway.
“Although our findings suggest that probiotics do not help prevent gastrointestinal colonization with drug-resistant organisms in critically ill patients, further study is necessary in this field,” Kwon said.
To that end, Kwon is part of a Washington University research team evaluating probiotics in hospitalized patients who are not in ICUs.
Washington University School of Medicine’s 2,100 employed and volunteer faculty physicians also are the medical staff of Barnes-Jewish and St. Louis Children’s hospitals. The School of Medicine is one of the leading medical research, teaching and patient-care institutions in the nation, currently ranked sixth in the nation by U.S. News & World Report. Through its affiliations with Barnes-Jewish and St. Louis Children’s hospitals, the School of Medicine is linked to BJC HealthCare.