Inflammatory bowel disease (IBD) afflicts 1.6 million people in the United States, causing abdominal pain, diarrhea, constipation, rectal bleeding and other potentially debilitating symptoms.
Crohn’s disease and ulcerative colitis are the most common forms of IBD, an autoimmune condition that is thought to develop based on genetic and environmental factors.
The microbes that colonize the gut are likely an important environmental factor. In most cases, these bacteria are beneficial to humans. However, certain bacteria can get through the protective layer of mucus that covers the inner lining of the gut.
Scientists have theorized that under the right conditions, such bacteria burrow their way into the gut lining, inciting immune cells to attack and harm the intestine.
But researchers at Washington University School of Medicine in St. Louis have found that these battles can start in a very different manner, a finding that could lead to better treatments for IBD. Working in mice, they showed that particular bacteria aren’t the direct fighters in this conflict; instead, the bacteria produce small particles that can get into the lining of the gut and provoke an aggressive response from the immune system.
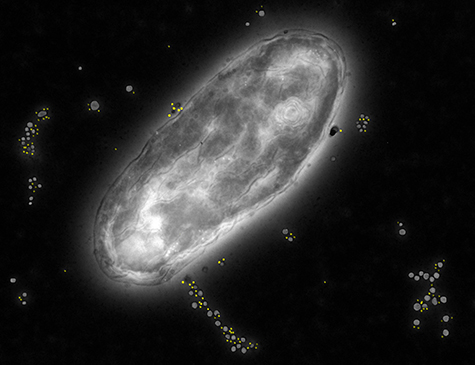
“You can compare these particles, which are known as vesicles, to fighter jets being released from a bacterial mothership,” said co-author Christina Hickey, MD, a clinical fellow. “Having a more accurate picture of how these jets trigger the onset of an attack should help us devise better ways to help prevent IBD symptoms.”
The researchers’ results highlight a bacterial enzyme that could be a target for IBD treatments.
The study appears May 13 in Cell Host & Microbe.
As part of the study, co-authors Thad Stappenbeck, MD, PhD, professor of pathology and immunology, and Paul Allen, PhD, the Robert L. Kroc Professor of Pathology and Immunology, worked with mice they genetically altered to develop a condition similar to very early onset IBD. This disorder, which can cause more severe symptoms than adult forms of the disease, typically is diagnosed before age 6. It often is caused by rare genetic mutations.
With Eric Martens, PhD, of the University of Michigan, the researchers studied a bacterial species known to cause colon inflammation in the mice. They suspected that Bacteroides thetaiotaomicron (B. theta) degrades the mucus that lines the interior of the gut, enabling the bacteria to enter the gut tissue, encounter immune cells and provoke an immune response that leads to the intestinal inflammation that characterizes IBD.
Instead, to their surprise, they found that the bacteria remain in the gut, while vesicles made by the bacteria make their way into the gut tissue. These vesicles are tiny spherical pockets that pinch off from the bacteria’s outer membranes. The vesicles travel from the bacteria into the tissue of the host, where they interact with the immune cells.
“The immune cells don’t need to encounter the bacteria to cause inflammation — all they need to do is encounter the vesicles,” Stappenbeck said. “We didn’t realize that was possible, and we think this discovery could change our thinking about not just IBD but other autoimmune disorders and infectious diseases.”
The research showed that the contents of the particles included a bacterial protein that causes inflammation. According to the scientists, a drug that blocks this protein might help prevent vesicles from leaving the gut and contributing to IBD.