Scientists at Washington University School of Medicine in St. Louis have discovered what appears to be a potent stimulator of new bone growth. The finding could lead to new treatments for osteoporosis and other diseases that occur when the body doesn’t make enough bone.
Osteoporosis affects 55 percent of Americans age 50 and older. Of that age group, one in three women and one in 12 men are believed to have osteoporosis, a condition responsible for millions of fractures each year, mostly involving the hips, wrist or lower back vertebrae.
“We have been looking for new ways to stimulate bone formation,” said principal investigator Fanxin Long, PhD. “The tools we already have are very good at slowing the breakdown of bone, but we need better ways to stimulate new bone growth.”
Studying mice, Long focused on a pathway involved in bone formation. The so-called WNT proteins carry messages into cells and regulate embryonic and adult tissue in mammals, including humans. The WNT proteins enter cells from the outside and then can activate multiple pathways inside those cells.
Long’s team reports Jan. 30 in the journal PLOS Genetics that a specific member of the WNT family of proteins dramatically enhances bone formation, and it works through a mechanism that has not been well-studied in bone before.
It’s called the mTOR pathway, and it interprets a cell’s surrounding environment, and nutritional and energy status.
“By analyzing that information, mTOR can determine whether a cell should go into a mode to make lots of stuff, like proteins or, in this case, new bone,” explained Long, a professor of orthopaedic surgery. “Bone formation is an energetically expensive process, so it makes sense that some regulator would tell a cell whether there is sufficient energy and material to manufacture new bone.”
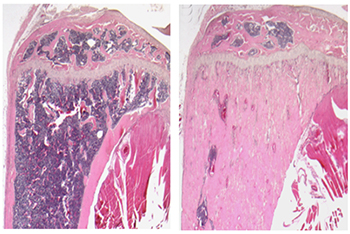
Long and his colleagues studied mice that made either normal levels or an extra amount of WNT proteins. They found that a particular WNT protein, WNT7B, is a potent stimulator of bone formation in mice. Mice engineered to make additional WNT7B manufactured new bone at much higher rates than normal mice.
The researchers also found that the protein created more bone by greatly increasing the number of bone-manufacturing cells in the mice. Our bones are in a constant state of flux as the number of bone-making (osteoblast) cells fluctuates, while the number of bone-degrading (osteoclast) cells also adjusts.
The WNT7B protein had no effect on the total activity of bone-degrading osteoclasts but substantially increased the number of bone-building osteoblast cells. And it did so by stimulating the mTOR pathway.
“It’s still early, but our finding seems to point out that activating the mTOR pathway may be a good way to stimulate bone growth,” said Long, also a professor of medicine and of developmental biology. “This is a new twist because much of the current focus in mTOR-related drug development has been on compounds that inhibit the pathway to shut down cancer cells.”
Drugs that inhibit the mTOR pathway also are used to suppress the immune response in patients undergoing organ transplants. Interestingly, bone problems are common in those patients.
“Many develop bone problems within a few months of receiving transplants because of the heavy doses of immunosuppressors they receive,” Long explained. “Scientists have not looked carefully at how drugs used to prevent organ rejection can have a detrimental effect on bone, but our study would suggest that if those drugs inhibit mTOR, they could disrupt bone formation.”
Next, Long plans to look more deeply at the mechanism through which the WNT proteins instruct bone cells to activate mTOR and stimulate bone growth. His goal is to learn what happens farther along in that pathway to create new bone. If more specific targets can be identified in the bone-formation process, drugs potentially could be developed to stimulate bone formation in people with osteoporosis without causing unwanted side effects.
Funding for this research comes from the National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS) and the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) of the National Institutes of Health (NIH).
NIH grant numbers R01 AR060456, DK065789 and P30 AR057235.
Chen J, Tu X, Esen E, Joeng KS, Lin C, Arbeit JM, Ruegg MA, Hall MN, Ma L, Long F. WNT7B promotes bone formation in part through mTORC1. PLoS Genetics, Jan. 30, 2014.
http://www.plosgenetics.org/doi/pgen.1004145
Washington University School of Medicine’s 2,100 employed and volunteer faculty physicians also are the medical staff of Barnes-Jewish and St. Louis Children’s hospitals. The School of Medicine is one of the leading medical research, teaching and patient-care institutions in the nation, currently ranked sixth in the nation by U.S. News & World Report. Through its affiliations with Barnes-Jewish and St. Louis Children’s hospitals, the School of Medicine is linked to BJC HealthCare.