When bees sting, they pump poison into their victims. Now the toxin in bee venom has been harnessed to kill tumor cells by researchers at Washington University School of Medicine in St. Louis. The researchers attached the major component of bee venom to nano-sized spheres that they call nanobees.
In mice, nanobees delivered the bee toxin melittin to tumors while protecting other tissues from the toxin’s destructive power. The mice’s tumors stopped growing or shrank. The nanobees’ effectiveness against cancer in the mice is reported in advance online publication Aug. 10 in the Journal of Clinical Investigation.
“The nanobees fly in, land on the surface of cells and deposit their cargo of melittin which rapidly merges with the target cells,” says co-author Samuel Wickline, M.D., who heads the Siteman Center of Cancer Nanotechnology Excellence at Washington University. “We’ve shown that the bee toxin gets taken into the cells where it pokes holes in their internal structures.”
Melittin is a small protein, or peptide, that is strongly attracted to cell membranes, where it can form pores that break up cells and kill them.
“Melittin has been of interest to researchers because in high enough concentration it can destroy any cell it comes into contact with, making it an effective antibacterial and antifungal agent and potentially an anticancer agent,” says co-author Paul Schlesinger, M.D., Ph.D., associate professor of cell biology and physiology. “Cancer cells can adapt and develop resistance to many anticancer agents that alter gene function or target a cell’s DNA, but it’s hard for cells to find a way around the mechanism that melittin uses to kill.”
The scientists tested nanobees in two kinds of mice with cancerous tumors. One mouse breed was implanted with human breast cancer cells and the other with melanoma tumors. After four to five injections of the melittin-carrying nanoparticles over several days, growth of the mice’s breast cancer tumors slowed by nearly 25 percent, and the size of the mice’s melanoma tumors decreased by 88 percent compared to untreated tumors.
The researchers indicate that the nanobees gathered in these solid tumors because tumors often have leaky blood vessels and tend to retain material. Scientists call this the enhanced permeability and retention effect of tumors, and it explains how certain drugs concentrate in tumor tissue much more than they do in normal tissues.
But the researchers also developed a more specific method for making sure nanobees go to tumors and not healthy tissue by loading the nanobees with additional components. When they added a targeting agent that was attracted to growing blood vessels around tumors, the nanobees were guided to precancerous skin lesions that were rapidly increasing their blood supply. Injections of targeted nanobees reduced the extent of proliferation of precancerous skin cells in the mice by 80 percent.
Overall, the results suggest that nanobees could not only lessen the growth and size of established cancerous tumors but also act at early stages to prevent cancer from developing.
“Nanobees are an effective way to package the useful, but potentially deadly, melittin, sequestering it so that it neither harms normal cells nor gets degraded before it reaches its target,” Schlesinger says.
If a significant amount of melittin were injected directly into the bloodstream, widespread destruction of red blood cells would result. The researchers showed that nanoparticles protected the mice’s red cells and other tissues from the toxic effects of melittin. Nanobees injected into the bloodstream did not harm the mice. They had normal blood counts, and tests for the presence of blood-borne enzymes indicative of organ damage were negative.
When secured to the nanobees, melittin is safe from protein-destroying enzymes that the body produces. Although unattached melittin was cleared from the mice’s circulation within minutes, half of the melittin on nanobees was still circulating 200 minutes later. Schlesinger indicates that is long enough for the nanobees to circulate through the mice’s bloodstream 200 times, giving them ample time to locate tumors.
“Melittin is a workhorse,” says Wickline, also professor of medicine in the Cardiovascular Division and professor of physics, of biomedical engineering and of cell biology and physiology. “It’s very stable on the nanoparticles, and it’s easily and cheaply produced. We are now using a nontoxic part of the melittin molecule to hook other drugs, targeting agents or imaging compounds onto nanoparticles.”
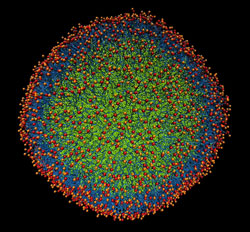
The core of the nanobees is composed of perfluorocarbon, an inert compound used in artificial blood. The research group developed perfluorocarbon nanoparticles several years ago and have been studying their use in various medical applications, including diagnosis and treatment of atherosclerosis and cancer. About six millionths of an inch in diameter, the nanoparticles are large enough to carry thousands of active compounds, yet small enough to pass readily through the bloodstream and to attach to cell membranes.
“We can add melittin to our nanoparticles after they are built,” Wickline says. “If we’ve already developed nanoparticles as carriers and given them a targeting agent, we can then add a variety of components using native melittin or melittin-like proteins without needing to rebuild the carrier. Melittin fortunately goes onto the nanoparticles very quickly and completely and remains on the nanobee until cell contact is made.”
The flexibility of nanobees and other nanoparticles made by the group suggests they could be readily adapted to fit medical situations as needed. The ability to attach imaging agents to nanoparticles means that the nanoparticles can give a visible indication of how much medication gets to tumors and how tumors respond.
“Potentially, these could be formulated for a particular patient,” Schlesinger says. “We are learning more and more about tumor biology, and that knowledge could soon allow us to create nanoparticles targeted for specific tumors using the nanobee approach.”
Soman NR, Baldwin SL, Hu G, Marsh JN, Lanza GM, Heuser JE, Arbeit JM, Wickline SA, Schlesinger PH. Molecularly targeted nanocarriers deliver the cytolytic peptide melittin specifically to tumor cells in mice, reducing tumor growth. Journal of Clinical Investigation. August 10, 2009 (advance online publication).
Funding from the National Institutes of Health and the American Heart Association supported this research.
Washington University School of Medicine’s 2,100 employed and volunteer faculty physicians also are the medical staff of Barnes-Jewish and St. Louis Children’s hospitals. The School of Medicine is one of the leading medical research, teaching and patient care institutions in the nation, currently ranked third in the nation by U.S. News & World Report. Through its affiliations with Barnes-Jewish and St. Louis Children’s hospitals, the School of Medicine is linked to BJC HealthCare.
Siteman Cancer Center is the only federally designated Comprehensive Cancer Center within a 240-mile radius of St. Louis. Siteman Cancer Center is composed of the combined cancer research and treatment programs of Barnes-Jewish Hospital and Washington University School of Medicine. Siteman has satellite locations in West County and St. Peters, in addition to its full-service facility at Washington University Medical Center on South Kingshighway.