The National Institutes of Health (NIH) has awarded scientists at Washington University School of Medicine in St. Louis four grants totaling $19 million to explore the trillions of microbes that inhabit the human body and determine how they contribute to good health and disease.
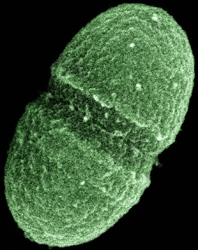
The grants are part of the Human Microbiome Project, an ongoing, ambitious effort to catalog the bacteria, viruses, fungi and other microorganisms that naturally coexist in or on the body. In all, the NIH today announced $42 million in grant awards to 12 U.S. institutions that expand the scope of the microbiome project.
The largest chunk – $16 million – goes to Washington University’s Genome Center, which played a central role in the initial phase of the project. In the new four-year effort, WU genome scientists, led by George Weinstock, Ph.D., will decode the DNA of about 400 microbes in collaboration with scientists at three other large-scale DNA sequencing centers. This information will then be used to catalog the microbes found in samples from healthy human volunteers to find out which microbes live in various ecological niches of the body. Samples will be collected from the mouth, skin, nose, vagina and digestive tract.
“We can’t really understand human health and disease without understanding the massive community of microorgansims we carry around with us,” says Weinstock, professor of genetics and associate director of the Genome Center. “This effort will tell us which microbes are present in certain areas of the body and what they are doing there. Ultimately, this information will change how we think about and treat many illnesses.”
Many scientists consider humans as superorganisms, a synergistic community of both human and bacterial cells that is more than the sum of its parts. The microbial cells in the human body are major players: they outnumber human cells by at least 10 to 1. Moreover, our bodies carry more than 100 times as many microbial genes as human genes. These microbes contribute essential functions that humans have either lost or never been able to perform on their own, such as synthesizing certain vitamins, digesting complex sugars, or helping the body to ward off harmful disease-causing microorganisms.
Washington University researchers also received another $3 million for three pilot demonstration projects that investigate the link between changes in microbial communities and certain diseases. These one-year projects involve sampling the microbiomes of both healthy and ill volunteers. By comparing differences in microbial communities between the two groups, researchers hope to determine how microbes influence the risk of disease.
Gastroenterologist Ellen Li, Ph.D., professor of medicine, is evaluating whether patients with Crohn’s disease, a gastrointestinal illness that causes severe abdominal pain and diarrhea, have a genetic makeup that alters the types of microbes that colonize the intestinal tract. She and her colleagues suspect that mutations in the human genome combine with changes in the composition of intestinal microbes to cause the inflammation that is the hallmark of the disease.
Gregory Storch, M.D., the Ruth L. Siteman Professor of Pediatrics, is working to uncover the full spectrum of viruses that cause sudden, high fevers in otherwise healthy children. His team will analyze blood samples and respiratory and gastrointestinal secretions from children with fever and healthy children to look for both known and new viruses. This information provides as a basis for understanding how viruses may contribute to fevers that cannot be traced to a recognized cause. The scientists also will carry out similar studies in children whose immune systems are suppressed, either by HIV/AIDS and other illnesses or by medications related to organ and stem cell transplants.
Phil Tarr, M.D., the Melvin E. Carnahan Professor in Pediatrics and head of pediatric gastroenterology, is investigating whether necrotizing enterocolitis, a devastating gastrointestinal illness that primarily affects premature infants, is linked to microbes in the intestinal tract. The condition affects about 10 percent of premature babies, usually in the first month of life, and is fatal in 15 to 30 percent of cases. Tarr and his colleagues are collecting fecal samples from premature babies to identify and quantify differences between the microbial communities of the infants who develop the illness and those who do not. This information may provide a foundation for developing ways to prevent or cure the illness.
Washington University’s Genome Center will also collaborate on two additional pilot demonstration projects. One probes the link between the skin microbiome and acne in a project led by researchers at the University of California at Los Angeles. The other examines the microbiome of the urethra in adolescent males and its relationship to puberty, sexual activity and sexually transmitted diseases.
The pilot demonstration projects will be reviewed after one year to assess their progress in showing a relationship between a particular disease and the microbiome of a body site. Projects with encouraging results may be selected for expansion and additional funding.
“Washington University is becoming a leader in a field that combines a high level of expertise in genome sequencing with physicians’ intimate knowledge of disease,” Weinstock says. “This large-scale effort will open doors in many areas of medicine to improve our understanding of good health and the treatment and prevention of disease.”
Washington University School of Medicine’s 2,100 employed and volunteer faculty physicians also are the medical staff of Barnes-Jewish and St. Louis Children’s hospitals. The School of Medicine is one of the leading medical research, teaching and patient care institutions in the nation, currently ranked third in the nation by U.S. News & World Report. Through its affiliations with Barnes-Jewish and St. Louis Children’s hospitals, the School of Medicine is linked to BJC HealthCare.