Heart surgeons at Washington University School of Medicine in St. Louis have helped usher in a new era in the surgical treatment of atrial fibrillation. Using radiofrequency devices — rather than a scalpel — they’ve greatly shortened the surgery and made it significantly easier to perform.
“Because of the devices, the procedure — called the Cox-Maze procedure — has gone from an operation that hardly anyone was doing to one that 80 to 90 percent of U.S. heart surgeons are now performing,” says Ralph J. Damiano Jr., M.D., the John Shoenberg Professor of Surgery and chief of cardiac surgery at the School of Medicine and a cardiac surgeon at Barnes-Jewish Hospital.
Adults older than 40 have a 25 percent risk of eventually developing atrial fibrillation in which the upper chambers of the heart twitch rapidly instead of contracting fully and regularly. The condition can lead to stroke or heart failure.
For some patients, medications can control the abnormal heart rhythms and the risk of clotting associated with atrial fibrillation, but they do not cure the disorder. The Cox-Maze procedure has a greater than 90 percent cure rate.
Damiano and his colleagues have played a vital role in the development and testing of radiofrequency devices for treating atrial fibrillation. The devices deliver high-energy radiofrequency waves to heart tissue and very quickly create scars or ablations, which replace most of the complex incisions required by the Cox-Maze procedure. The ablations disrupt the atria’s abnormal electrical activity and normalize heart rhythm.
The research team found that surgeons needed to apply the devices for only a few seconds at a time to get effective ablation of the atrial wall, and the devices caused no injury to surrounding tissue. The time needed for the procedure went from more than 90 minutes to about 30 minutes.
The modified Cox-Maze procedure eliminated atrial fibrillation in over 90 percent of patients in a recent study, a number that compares favorably to the outcomes of the traditional cut-and-sew procedure. About three-quarters of patients treated no longer need drugs to prevent abnormal heart rhythms or excessive blood clotting, Damiano says.
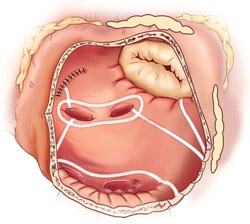
The Cox-Maze procedure is named for James Cox, M.D., former director of Washington University’s division of cardiothoracic surgery, who led the St. Louis research group that developed the procedure in 1987. The procedure — which revolutionized treatment of atrial fibrillation — calls for ten precisely placed incisions in the upper chambers of the heart. The incisions are then sewn up and eventually form scars in the atrial tissue.
The scar tissue stops atrial fibrillation by interfering with chaotic electrical signals that cause the atria to contract irregularly. By placing roadblocks in the way of these misplaced electrical impulses, the Cox-Maze procedure redirects them down their normal route so that they stimulate regular heartbeats.
The clamp-like jaws of the radiofrequency ablation devices latch onto a section of heart muscle and deliver a thin, focused line of energy that heats and ablates the tissue. Ablation with the devices can replace all but two small incisions that would typically be made during a traditional Cox-Maze procedure.

“We’ve not only reduced the time needed for the procedure, we’ve made the procedure easier to perform,” Damiano says. “In addition to eliminating most of the incisions, the radiofrequency ablation clamp removes the potential for error by monitoring when the lesion goes all the way through the tissue and automatically shutting the power off at that point.”
By simplifying the Cox-Maze surgery, the method will make the procedure available to more patients. “This has made it possible to offer this curative operation to almost everyone coming for heart surgery who has chronic atrial fibrillation,” Damiano says.
Other devices exist to create the Cox-Maze lesions — these use microwaves, lasers, ultrasound or freezing. Damiano believes that the type of device used at the School of Medicine is superior because other types of devices may not be as consistent or as fast and can cause collateral damage to other areas of the heart.
Damiano and colleagues are now working to develop a device that will make the Cox-Maze procedure even less invasive. The device would allow surgeons to perform the procedure on the beating heart and do away with the need to stop the heart and place the patient on a heart-lung machine. Heart-lung machines can introduce the potential for stroke or organ failure with extended use.
“We’ve made the first big step: we’ve taken a very complicated operation and made it simpler. We’ve tremendously decreased morbidity and virtually eliminated mortality,” Damiano says. “Now we are aggressively working on a device that would allow us to do the full set of Cox-Maze lesions without using a heart-lung machine.”
Melby SJ, Zierer AZ, Bailey MS, Cox JL, Lawton, JS, Munfakh N, Crabtree TD, Moazami N, Huddleston CB, Moon MR, Damiano RJ Jr. A new era in the surgical treatment of atrial fibrillation: The impact of ablation technology and lesion set on procedural efficacy. Annals of Surgery 2006;244(4);583-592.
Funding from the National Institutes of Health supported this research.
Ralph J. Damiano Jr. is a consultant for Atricure Inc. and Medtronic Inc., developers of the devices used in the study.
Washington University School of Medicine’s full-time and volunteer faculty physicians also are the medical staff of Barnes-Jewish and St. Louis Children’s hospitals. The School of Medicine is one of the leading medical research, teaching and patient care institutions in the nation, currently ranked fourth in the nation by U.S. News & World Report. Through its affiliations with Barnes-Jewish and St. Louis Children’s hospitals, the School of Medicine is linked to BJC HealthCare.