A multitude of genes have been linked to the development of Alzheimer’s disease. Specifically how those genes might influence the progression of neurodegeneration remains something of a black box though, in part because of the challenges of examining in molecular detail the brain of a living patient.
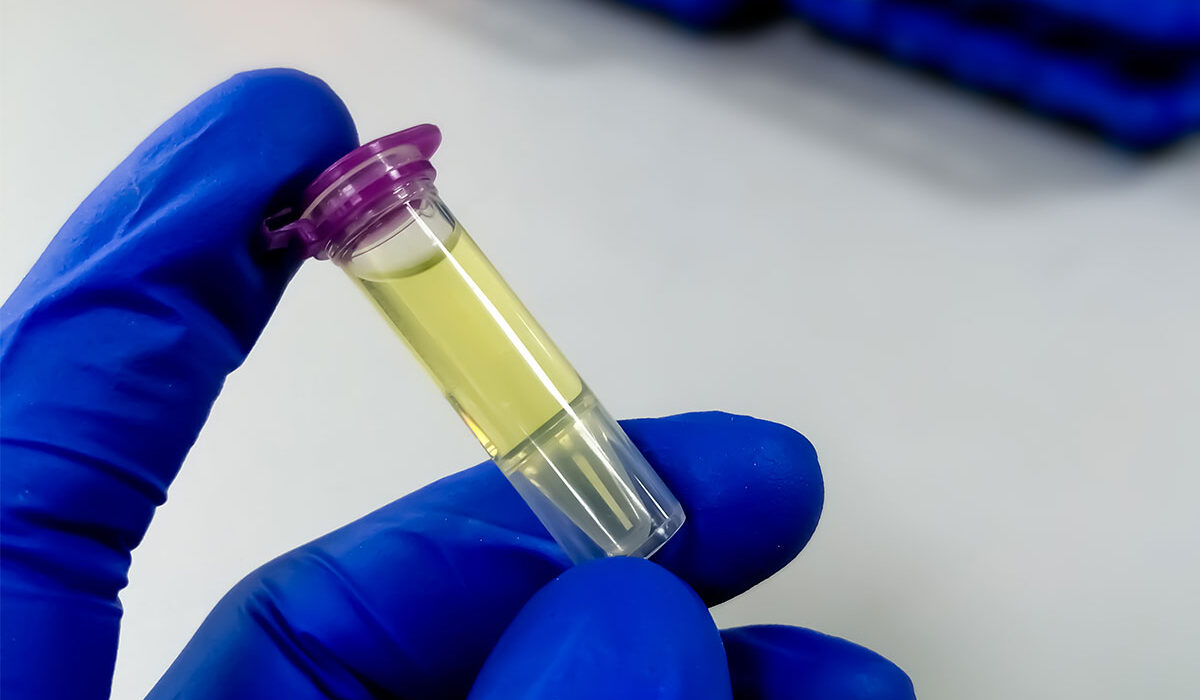
Using cerebrospinal fluid (CSF) collected from living patients, a team of researchers at Washington University School of Medicine in St. Louis has for the first time linked disease-related proteins and genes to identify specific cellular pathways responsible for Alzheimer’s genesis and progression. Because these proteins were gathered from CSF, they are a good proxy for activity in the brain, and several of them may be potential targets for therapies.
The findings are available in Nature Genetics.
The use of patients’ CSF is a step forward for such studies and may be the best way to acquire relevant samples that help map out the constellation of protein activity, known as the proteome, said Carlos Cruchaga, the Barbara Burton and Reuben Morriss III professor of psychiatry and director of the NeuroGenomics and Informatics Center at WashU Medicine.
“Our goal is to identify risk-linked and protective genes, and also identify the causal role they play,” Cruchaga said. “To do that, we need to study human-derived data. That is why we decided to do a large proteomic study of cerebrospinal fluid, because we know that CSF is a good representation of the pathology of the disease.”
Cruchaga explained that similar investigations have relied on brain tissues collected postmortem, and therefore only provide information about the later stages of Alzheimer’s. Other studies have looked at blood plasma, which is not specific to the tissues affected by the disease.
In the past decade and a half of researching Alzheimer’s disease, scientists have increased the number of regions of our genome known to be associated with the condition from 10 to nearly 80. However, knowing the gene or region of DNA associated with the disease is only the first step. Linking an individual’s proteomic profile – that is, which proteins are active and to what degree – to their genetic code establishes a holistic view of the cellular activities in the brain. By comparing CSF samples from people with and without Alzheimer’s disease, the researchers could then identify which cellular pathways are dysfunctional.
“Sometimes within a region of DNA known to be associated with Alzheimer’s there are many genes, and we don’t know which of those genes are driving the medical condition,” Cruchaga said. “By adding the proteins to the analysis, we can determine the gene driving the association, determine the molecular pathway that they are part of, as well as to identify novel protein-to-protein interactions that otherwise will not be possible.”
Cruchaga and his collaborators had access to a rich database of information through the Knight-ADRC and the Dominantly Inherited Alzheimer Network (DIAN), which are based at WashU Medicine, as well as other studies through their collaborators. These studies were also able to provide the genetic information and CSF samples of 3,506 individuals, both healthy donors and those with Alzheimer’s disease.
The team cross-referenced proteomic data from the CSF samples with existing studies that had identified areas of the genome correlated with Alzheimer’s. From this process, they narrowed in on 1,883 proteins of the 6,361 in the CSF proteomic atlas. The investigators used three different established statistical analyses that can identify with high confidence genes and proteins that are part of the biological pathways leading to the disease. With this technique, they determined that 38 proteins are likely to have causal effects in Alzheimer’s progression; 15 of these can be targeted by medicines.
“The novelty and the strength of this analysis is that we have defined proteins that modify risk,” Cruchaga said. “So now that we have the causal steps, we can establish where the steps are leading to in the brain.”
The immediate implications for understanding and developing treatments for Alzheimer’s from this study are significant, but Cruchaga said he believes that CSF proteomics may yield a treasure trove of information for many neurological conditions, ranging from Parkinson’s disease to schizophrenia.
“That’s the power of this approach — once you have an atlas of genetic variants, and that of the protein levels, you can apply this to any disease,” he said.
Proteins are not the only key to unlocking these conditions to be found in the CSF. Cruchaga also is investigating the potential of metabolites — substances released by cells when breaking down other compounds as part of their routine processes that are also found in CSF. In a separate paper, also published in Nature Genetics, he and his collaborators demonstrated the promise of this approach and reported associations between specific metabolites and conditions including Parkinson’s disease, diabetes and dementia.
Western D, Timsina J, Wang L, Wang C, Yang C, Phillips B, Wang Y, Liu M, Ali M, Beric A, Gorijala P, Kohlfeld P, Budde J, Levey AI, Morris JC, Perrin RJ, Ruiz A, Marquié M, Boada M, de Rojas I, Rutledge J, Oh H, Wilson EN, Le Guen Y, Reus LM, Tijms B, Jelle Visser P, van der Lee SJ, Pijnenburg YAL, Teunissen CE, del Campo Milan M, Alvarez I, Aguilar M, Dominantly Inherited Alzheimer Network (DIAN), the Alzheimer’s Disease Neuroimaging Initiative (ADNI), Greicius MD, Pastor P, Pulford DJ, Ibanez l, Wyss-Coray T, Sung YJ, Cruchaga C. Proteogenomic analysis of human cerebrospinal fluid identifies neurologically relevant regulation and implicates causal proteins for Alzheimer’s disease Nature Genetics. Nov. 11, 2024. DOI: 10.1038/s41588-024-01972-8
Cruchaga has received research support from GSK and Eisai. The funders of the study had no role in the collection, analysis or interpretation of data; in the writing of the report; or in the decision to submit the paper for publication. Cruchaga is a member of the advisory board of Circular Genomics and owns stocks in this company.
This work was supported by grants from the National Institutes of Health (NIH), R01AG044546, P01AG00399, RF1AG053303, RF1AG058501, U01AG058922, RF1AG074007, R00AG062723, P30 AG066515, NIH P30AG066444, P01AG03991, P01AG026276 the Chan Zuckerberg Initiative, the Michael J. Fox Foundation, the Department of Defense W81XWH2010849, the Alzheimer’s Association Zenith Fellows Award ZEN-22-848604, Bright Focus Foundation A2021033S. Alzheimer Nederland WE.03-2018-05, Selfridges Group Foundation NR170065. GlaxoSmithKline (GSK) provided funding to support the analyses performed in this study. The Dominantly Inherited Alzheimer’s Network is supported by U19AG032438, SG-20-690363-DIAN, ADNI U01 AG024904 Department of Defense W81XWH-12-2-0012). The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Wang C, Yang C, Western D, Ali M, Wang Y, Phuah C-L, Budde J, Wang L, Gorijala P, Timsina J, Ruiz A, Pastor P, Fernandez MV, Dominantly Inherited Alzheimer Network (DIAN), The Alzheimer’s Disease Neuroimaging Initiative (ADNI), Panyard DJ, Engelman CD, Deming Y, Boada M, Cano A, Garcia-Gonzalez P, Neill R, Graff-Radford NR, Mori H, Lee J-H, Perrin RJ, Ibanez L, Sung YJ, Cruchaga C. Genetic architecture of cerebrospinal fluid and brain metabolite levels and the genetic colocalization of metabolites with human traits. Nature Genetics. Nov. 11, 2024. DOI: 10.1038/s41588-024-01973-7
Cruchaga has received research support from GSK and EISAI and is a member of the advisory board of Circular Genomics and owns stocks.
This work was supported by grants from the National Institutes of Health (NIH; R01AG044546,P01AG003991, RF1AG053303, RF1AG058501, U01AG058922, RF1AG074007, R01/ RF1AG054047, the Chan Zuckerberg Initiative, the Michael J. Fox Foundation, the Department of Defense LI-W81XWH2010849, the Alzheimer’s Association Zenith Fellows Award ZEN-22-848604, and an anonymous foundation. Recruitment and clinical characterization of research participants at were supported by NIH P30AG066444, P01AG03991, P01AG026276.
Data collection and sharing was supported by the DIAN U19AG032438 and funded by the National Institute on Aging (NIA), the Alzheimer’s Association SG-20-690363-DIAN, ADNI NIH grant U01 AG024904and DOD ADNI W81XWH-12-2-0012. Further support came from the Spanish Ministry of Science, Innovation and Universities FJC2018-036012-I, Instituto de Salud Carlos III (ISCIII) CD22/00125, Proyectos de Generación de Conocimiento PID2021-122473OA-I00.
The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
About Washington University School of Medicine
WashU Medicine is a global leader in academic medicine, including biomedical research, patient care and educational programs with 2,900 faculty. Its National Institutes of Health (NIH) research funding portfolio is the second largest among U.S. medical schools and has grown 56% in the last seven years. Together with institutional investment, WashU Medicine commits well over $1 billion annually to basic and clinical research innovation and training. Its faculty practice is consistently within the top five in the country, with more than 1,900 faculty physicians practicing at 130 locations and who are also the medical staffs of Barnes-Jewish and St. Louis Children’s hospitals of BJC HealthCare. WashU Medicine has a storied history in MD/PhD training, recently dedicated $100 million to scholarships and curriculum renewal for its medical students, and is home to top-notch training programs in every medical subspecialty as well as physical therapy, occupational therapy, and audiology and communications sciences.
Originally published on the WashU Medicine website