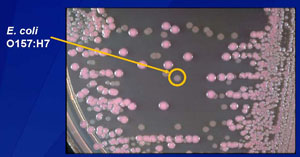
E. coli O157:H7 infection has been caused by eating undercooked hamburger, sprouts, unpasteurized fruit juices, dry-cured salami, lettuce, game meat and unpasteurized milk products, as well as exposure to contaminated water and contact with cattle.
Centers for Disease Control and Prevention
Infection with E. coli bacteria can wreak havoc in children, leading to bloody diarrhea, fever and kidney failure.
But giving children intravenous fluids early in the course of an E. coli O157:H7 infection appears to lower the odds of developing severe kidney failure, according to researchers at Washington University School of Medicine in St. Louis and other institutions. The results are published online July 22, 2011, in the Archives of Pediatric and Adolescent Medicine.
Children infected with E. coli O157:H7 have a high risk of hemolytic uremic syndrome (HUS), the most common cause of short-term, sudden-onset pediatric kidney failure. About 15 percent to 20 percent of children with this type of E. coli infection develop HUS. While most children recover and their kidneys heal, the syndrome can be lethal and may cause permanent kidney damage.
E. coli O157:H7 begins with diarrhea and severe abdominal pain and often progresses to bloody diarrhea. Kidney failure occurs because this strain of E. coli O157:H7 makes toxins, called Shiga toxins, that injure blood vessels. The kidneys are especially susceptible to the reduced blood flow that results from this injury. More than half of children with HUS develop kidney failure so severe that dialysis is required.

“HUS is like a heart attack to the kidneys,” says Christina Ahn Hickey, MD, a third-year pediatrics resident at Washington University School of Medicine in St. Louis and St. Louis Children’s Hospital and the first author on the study. “What we’re trying to do is make sure the kidneys get enough blood flow. By giving intravenous fluids, we try to keep those kidneys working and to keep these children urinating. We think this will have a substantial impact on reducing the severity of kidney failure in these kids.”
E. coli O157:H7 infection has been caused by eating undercooked hamburger, sprouts, unpasteurized fruit juices, dry-cured salami, lettuce, game meat and unpasteurized milk products, as well as exposure to contaminated water and contact with cattle. E. coli O157:H7 is the most common cause of acute kidney failure in otherwise healthy children in the developed world.
Hickey studied 50 children under 18 years old who were treated for diarrhea-associated HUS at 11 pediatric hospitals in the United States (St. Louis; Seattle; Sacramento, Calif.; Albuquerque, N.M.; Little Rock, Ark.; Milwaukee; Cincinnati and Columbus, Ohio; Indianapolis; and Memphis, Tenn.) and in Glasgow, Scotland. Her St. Louis collaborators were Robert J. Rothbaum, MD, the Centennial Professor of Pediatrics, and Anne M. Beck, MD, associate professor of pediatrics, both at Washington University School of Medicine.
In all, 68 percent of the children stopped urinating. Of the 25 patients who had received no intravenous fluids in the first four days of illness, 84 percent stopped urinating. But in the other 25 patients who were given IV fluids to keep their kidneys working, only 52 percent stopped urinating. Other factors did not seem to play a role, Hickey says.
“If a child is identified early as having an E. coli O157:H7 infection, we think that intravenous fluids can help protect the kidney and possibly help that child avoid dialysis,” Hickey says. “The important thing is for providers to identify the kids at risk for E. coli O157:H7 infection early.”
Intravenous fluids are more beneficial to children than oral fluids, Hickey says, because most of the children infected with E. coli O157:H7 are vomiting and having frequent bouts of diarrhea, so they cannot stay hydrated.
“To ensure that the kidneys get enough blood flow, we need to have sodium-containing fluid go straight to the blood vessels, and it’s faster and more effective to use an IV,” Hickey says.
Hickey says any child with bloody diarrhea needs to be seen by a health-care provider immediately.
“E. coli is very infectious,” she says. “It takes less than 1,000 organisms of E. coli to infect someone else. When a child has diarrhea, there are 10 million to 100 million pathogens in each gram of stool. It is really important to get them away from other children immediately, and hospitalization can serve as effective infection control.”
Phillip I. Tarr, MD, the Melvin E. Carnahan Professor of Pediatrics and director of the Division of Pediatric Gastroenterology, supervised Hickey on the study and is senior author of the paper.
“Christina coordinated this multicenter prospective study by herself,” he says. “She spoke to the families, collected and analyzed the data and wrote most of the manuscript, all as a medical student. This paper, appearing in the wake of the massive European outbreak caused by E. coli O104:H4, which also causes kidney failure and bloody diarrhea, is tragically timely. Because of her efforts, we will be able to manage children and adults with these infections more effectively and probably reduce the need for dialysis. It will be a landmark contribution to the field because we have no other interventions to offer infected patients.”
Hickey CA, Beattie TJ, Cowieson J, Miyashita Y, Strife CF, Frem JC, Peterson JM, Butani L, Jones DP, Havens PL, Patel HP, Wong CS, Andreoli SP, Rothbaum RJ, Beck AM, Tarr PI. Early Volume Expansion during Diarrhea and Relative Nephroprotection During Subsequent Hemolytic Uremic Syndrome. Archives of Pediatric and Adolescent Medicine, online July 22, 2011.
Funding from Christina Ahn Hickey’s Doris Duke Clinical Research Fellowship supported this research.
Washington University School of Medicine’s 2,100 employed and volunteer faculty physicians also are the medical staff of Barnes-Jewish and St. Louis Children’s hospitals. The School of Medicine is one of the leading medical research, teaching and patient care institutions in the nation, currently ranked fourth in the nation by U.S. News & World Report. Through its affiliations with Barnes-Jewish and St. Louis Children’s hospitals, the School of Medicine is linked to BJC HealthCare.