The cancer therapy known as CAR-T has revolutionized treatment of some blood cancers since it was introduced in 2017. The therapy uses genetically altered immune cells to home in on cancer cells and destroy them.
Now, studying mice with an autoimmune disease similar to multiple sclerosis (MS), researchers at Washington University School of Medicine in St. Louis have shown that the same approach can be used to eliminate unwanted cells that cause autoimmunity. The findings, available online in Science Immunology, extend the powerful tool of immunotherapy to a class of diseases that are often debilitating and difficult to treat.
“We were able to use CAR-T cells to eliminate just the immune cells that are causing the autoimmunity and not other immune cells you might need to protect against viruses or other infection,” said co-senior author Chyi-Song Hsieh, MD, PhD, the Alan A. and Edith L. Wolff Professor of Rheumatology and a professor of medicine and of pathology & immunology. “Our CAR-T cells were very effective at treating mice that have an MS-like disease.”
At the heart of CAR-T therapy are the immune system’s T cells, crucial elements of the body’s defense force. T cells respond to threats such as bacteria, viruses and cancerous cells by coordinating an immune assault and killing foreign organisms and infected or cancerous cells.
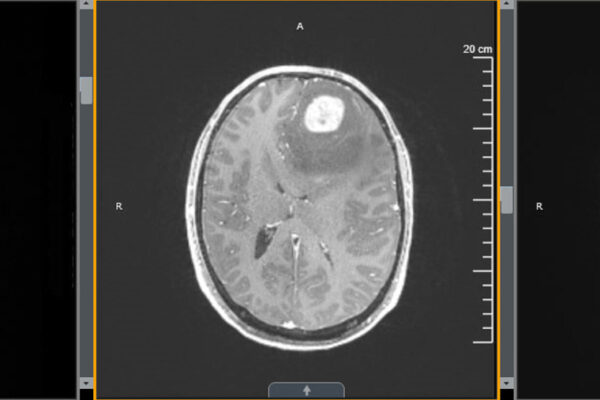
But every once in a while, T cells mistake healthy cells for infected cells and turn their weapons on the body’s own cells and tissues, triggering an autoimmune disease. MS is marked by rogue T cells that trigger the destruction of myelin, the protective covering over nerves. As myelin is eaten away, communication between the brain and spinal cord and the rest of the body becomes unreliable, and people begin experiencing symptoms such as fatigue, pain, tingling, vision problems and loss of coordination. Immunosuppressive drugs can quash the self-destructive activity of rogue T cells, but such drugs also suppress helpful T cells and put people at risk of severe infections.
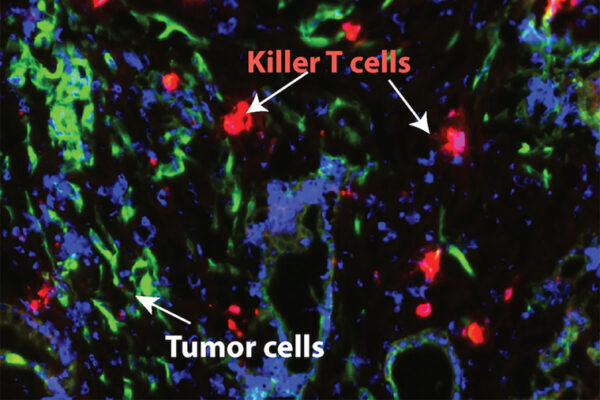
In CAR-T cancer therapies, doctors take a patient’s own T cells, modify them to recognize and vigorously attack his or her specific cancer, and then put them back in the body on a seek-and-destroy mission. Inspired by this approach, the researchers set out to create CAR-T cells equipped to seek out and destroy the rogue T cells that cause MS. The idea was to make CAR-T cells that would function akin to a police department’s internal affairs office, rooting out the bad apples in the T cells defense force while leaving good T cells in place to protect the body.
“Having MS can really erode your quality of life, and while current therapies slow down the course of the disease, they don’t cure it and they have side effects,” said co-senior author Gregory F. Wu, MD, PhD, an associate professor of neurology and of pathology & immunology. “I believe that this is a fully treatable disease, and CAR-T cells may be the way toward much better therapeutics.”
Along with Hsieh and Wu, the research team included co-authors Nathan Singh, MD, an assistant professor of medicine, and Takeshi Egawa, MD, PhD, an associate professor of pathology & immunology.
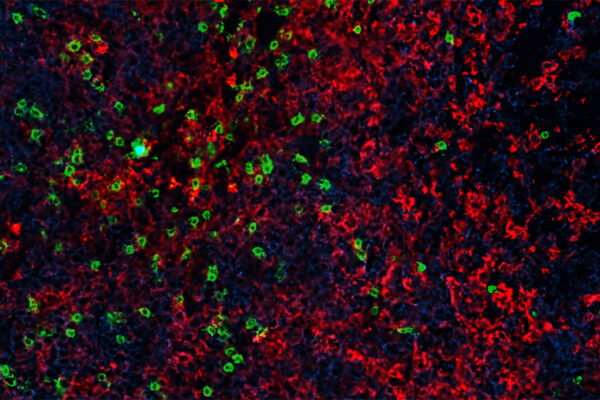
First, the researchers made some bait. They designed a molecule by combining a fragment of a protein found in myelin with a protein that activates T cells. Only T cells that target myelin — the bad apples, so to speak — would respond to this hybrid molecule. Then, they loaded the bait molecule onto a kind of T cell known as killer T cells. Any rogue T cells that took the bait would be eliminated by the killer T cells.
That was the idea, at least. To see whether it worked, the researchers turned to mice with an MS-like condition. Treating such mice with the engineered CAR-T cells prevented disease in those that had yet to develop problems, and reduced signs of disease in those that were already showing neurological effects.
“We’re working on improving the CAR-T cells, to get them to kill more efficiently and last longer so that we can get better treatment outcomes,” Hsieh said. “Right now, there’s no way to tell who is going to get MS or when, so preventing disease in people isn’t realistic, but we could treat it, and I think the CAR-T approach looks very promising.”
The beauty of the CAR-T approach is that by swapping out the protein fragment in the bait molecule, killer T cells can be redirected toward different rogue immune cells to treat different diseases.
“I see patients in the clinic who have a rare disease known as myelin oligodendrocyte glycoprotein (MOG) antibody disease that is very similar to MS,” Wu said. “Unlike MS, which is complicated, we know exactly what the target is in MOG antibody disease. I wish I could just get rid of these self-reactive cells for my patients, but we’ve had no way to do that. Now, we are working toward using the patient’s own immune cells to create CAR-T cells that would eliminate those self-reactive T cells.”
Yi J, Miller AT, Archambault AS, Jones AJ, Bradstreet TR, Bandla S, Hsu Y-S, Edelson BT, Zhou YW, Fremont DH, Ego T, Singh N, Wu GF, Hsieh C-S. Antigen-specific depletion of CD4+ T cells by CAR T cells reveals distinct roles of higher- and lower-affinity TCRs during autoimmunity. Science Immunology. Oct. 7, 2022. DOI:10.1126/sciimmunol.abo0777
This study was supported by the National Institute of Neurological Disorders and Stroke of the National Institutes of Health (NIH), grant number R01NS106289; the National Multiple Sclerosis Society, grant numbers RG-1802-30253 and RG- 2111-38724; the National Institute for Allergy and Infectious Diseases, grant numbers R01-AI07987 and R01AI165771; the National Cancer Institute, grant number K08CA237740; and the Wolff Professorship.
About Washington University School of Medicine
WashU Medicine is a global leader in academic medicine, including biomedical research, patient care and educational programs with 2,700 faculty. Its National Institutes of Health (NIH) research funding portfolio is the fourth largest among U.S. medical schools, has grown 54% in the last five years, and, together with institutional investment, WashU Medicine commits well over $1 billion annually to basic and clinical research innovation and training. Its faculty practice is consistently within the top five in the country, with more than 1,790 faculty physicians practicing at over 60 locations and who are also the medical staffs of Barnes-Jewish and St. Louis Children’s hospitals of BJC HealthCare. WashU Medicine has a storied history in MD/PhD training, recently dedicated $100 million to scholarships and curriculum renewal for its medical students, and is home to top-notch training programs in every medical subspecialty as well as physical therapy, occupational therapy, and audiology and communications sciences.