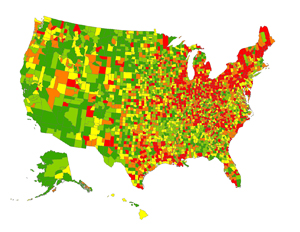
The largest epidemiological study of Parkinson’s disease in the United States has found that the disease is more common in the Midwest and the Northeast and is twice as likely to strike whites and Hispanics as blacks and Asians.
The study, based on data from 36 million Medicare recipients, is both the first to produce any significant information on patterns of Parkinson’s disease in minorities and to show geographic clusters for the condition.
“Finding clusters in the Midwest and the Northeast is particularly exciting,” says lead author Allison Wright Willis, M.D., assistant professor of neurology at Washington University School of Medicine in St. Louis. “These are the two regions of the country most involved in metal processing and agriculture, and chemicals used in these fields are the strongest potential environmental risk factors for Parkinson’s disease that we’ve identified so far.”
The results appear online in the journal Neuroepidemiology.
Parkinson’s disease is a common neurodegenerative condition that causes tremor, stiffness, slowness, mood and behavioral disorders, sleep problems and other symptoms. The disease is characterized by loss of dopamine, a compound involved in communication between brain cells.
According to Willis, genetic factors explain only a small percent of cases. Environmental factors are likely more common contributors and may include prolonged exposures to herbicides and insecticides used in farming or to metals such as copper, manganese and lead.
For the new study, Willis analyzed data on more than 450,000 cases of Parkinson’s disease per year over six years, 1995 and 2000-2005. Collectively, that data included information from more than 98 percent of all Americans 65 and older.
Willis found Asians and blacks developed Parkinson’s disease at half the rate of whites and Hispanics.
“We are going to try to learn more about why this is the case,” Willis says. “It could be that those with Asian or African ancestry have genes that help protect them from exposure to environmental factors that cause Parkinson’s disease, or they may have fewer exposures to those factors.”
Epidemiologists have long debated whether Parkinson’s disease is more prevalent in rural or urban areas, with some studies showing higher rates in cities and some in the countryside. Willis found the condition is more common in urban areas but concluded the comparison between the two rates offered little potential for insight into the disease.
“It’s always been an open question as to how to best define the terms ‘urban’ and ‘rural,’ ” Willis says. “Urban and rural is defined in many different and relatively arbitrary ways, and we came away convinced by our results that these distinctions have little to do with what is causing the disease.”
Willis and her colleagues plan further studies of how exposure to single or combined environmental factors influences disease risk.
“This was the largest descriptive epidemiological study yet to be conducted of Parkinson’s disease in the United States, and it has both given us some interesting new leads for the future research and reinforced some ideas we already had,” Willis says.
Wright Willis A, Evanoff BA, Lian M, Criswell SR, Racette BA. Geographic and ethnic variation in Parkinson disease: a population-based study of US Medicare beneficiaries. Neuroepidemiology, 2010;34:143-151
Funding from the National Institute for Environmental Health Science, the National Institute of Neurological Disorders and Stroke, and the National Center for Research Resources supported this research.
Washington University School of Medicine’s 2,100 employed and volunteer faculty physicians also are the medical staff of Barnes-Jewish and St. Louis Children’s hospitals. The School of Medicine is one of the leading medical research, teaching and patient care institutions in the nation, currently ranked third in the nation by U.S. News & World Report. Through its affiliations with Barnes-Jewish and St. Louis Children’s hospitals, the School of Medicine is linked to BJC HealthCare.


