There’s no cure for the so-called stomach flu, a group of highly contagious viruses that can hit with a vengeance, causing nausea, vomiting and diarrhea. Doctors’ standard advice: drink lots of fluids and let the virus run its course. Symptoms typically last only a couple of days, but they can be miserable ones.
Now, scientists at Washington University School of Medicine in St. Louis report they have identified the primary immune sensor that detects the presence of stomach viruses in the body. They show that the sensor – a protein called MDA-5 – triggers an immune response that revs up the body’s defenses to fight off the infection. This knowledge may help develop a treatment that prevents or reduces the infection, the researchers suggest in their study, published July 18 in the open-access journal PLoS Pathogens.
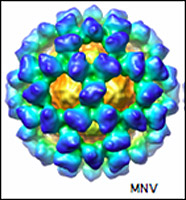
The stomach flu is technically not the flu at all: the flu virus only affects the respiratory tract. The stomach flu is known scientifically as a norovirus. Norovirus outbreaks are common in locations where people live close together, such as cruise ships, nursing homes, military bases and schools. Antibiotics are ineffective, because they fight bacteria, not viruses. Only recently have scientists been able to grow noroviruses in the laboratory and study them.
“Our research strongly indicates that MDA-5 is the primary sensor for norovirus infection, but the body’s ability to detect the virus is so important that it doesn’t just rely on one sensor,” says senior investigator Marco Colonna, Ph.D., professor of pathology and immunology. “We found that another protein sensor – TLR3 – serves as a back-up and there may be others that have not yet been discovered.”
The team demonstrated their work in mice but says the same proteins are likely responsible for detecting norovirus infection in humans. MDA-5, and to a lesser extent, TLR3, respond by causing other cells to release interferon, which shuts down production of the virus and initiates a full-scale immune attack. MDA-5 and TLR3 are both intracellular proteins.
The researchers suspected that these two proteins may be important in detecting noroviruses because they are known to be important in recognizing similar types of viral infections.
Lead author Stephen McCartney, a graduate student in Colonna’s lab, first found that cells in the test tube that lack the MDA-5 protein don’t mount an appropriate immune response against norovirus infection.
The team then investigated two groups of mice – one group was bred without the ability to produce MDA-5 and the other was bred to lack TLR3. Again, both groups of mice had a defective immune response against noroviruses. In particular, mice without MDA-5 had higher levels of norovirus in their bodies and a defect in the ability to signal other immune cells to respond. Mice that lacked TLR3 also had a decreased response to norovirus infection, the researchers noted.
Interestingly, some people have common variations of the MDA-5 gene that could make them more susceptible to norovirus infection, the researchers say. A norovirus treatment could be especially helpful to people who are more prone to the infection.
McCartney SA, Thackray LB, Gitlin L, Gilfillan S, Virgin HW, Colonna M. MDA-5 Recognition of a Murine Norovirus. PLoS Pathogens. http://www.plospathogens.org/doi/ppat.1000108
Funding from the Juvenile Diabetes Research Foundation supported this research.
Washington University School of Medicine’s 2,100 employed and volunteer faculty physicians also are the medical staff of Barnes-Jewish and St. Louis Children’s hospitals. The School of Medicine is one of the leading medical research, teaching and patient care institutions in the nation, currently ranked third in the nation by U.S. News & World Report. Through its affiliations with Barnes-Jewish and St. Louis Children’s hospitals, the School of Medicine is linked to BJC HealthCare.