Using a wide range of imaging techniques to visualize cancer in the body, radiology investigators at the Siteman Cancer Center at Barnes-Jewish Hospital and Washington University School of Medicine are expanding the boundaries of cancer detection, treatment and research. The strength of their efforts has received national recognition. For several years, Mallinckrodt Institute of Radiology at Washington University School of Medicine has ranked among the top three imaging programs in the United States in research grants received by the National Institutes of Health (NIH).

While Siteman’s imaging projects range widely, their goals are all the same: to better understand the molecular biology of a particular tumor. With that knowledge, scientists can begin to predict which cancer therapy will help each patient.
“This kind of ‘personalized imaging’ is unbelievably exciting,” says Michael Welch, PhD, associate director of oncologic imaging at Siteman and professor of radiology, chemistry, and molecular biology and pharmacology. “To be able to say in a very short time whether a therapy is working can change the approach to cancer treatment.”
In the area of nuclear imaging, professor of radiology Robert Mach, PhD, is working on new ways to identify rapidly growing cells that indicate an aggressive cancer. Mach’s research has shown that this kind of tissue contains more receptors than less actively growing tissue, so measuring receptor status is one way to assess cancer growth. This same measurement taken after therapy can also indicate whether treatment is working since cell proliferation will drop.
Now Mach is trying to pinpoint agents that work well with positron emission tomography (PET) – and more effectively than the most commonly used agent, fluorodeoxyglucose – in targeting the Sigma-2 receptor system, which exists in these highly proliferating tumors. He also is working to better understand another class of receptors, Caspase-3 receptors, that can indicate quickly whether therapy is effective.
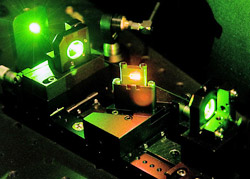
Optical imaging offers another exciting avenue of radiology research at Siteman, providing key advantages over other techniques. Since it does not involve radiation, it can be performed more frequently – especially important for children, whose radiation dose must be minimized. Optical imaging also is inherently sensitive and needs little enhancement by contrast agents.
Within this field, the optical imaging laboratory at Washington University School of Medicine has been very active. Samuel Achilefu, PhD, associate professor of radiology, is creating new optical probes, while physicist Joseph Culver, PhD, assistant professor of radiology, is developing instrumentation to use these probes for three-dimensional imaging and for imaging tissues beyond the reach of conventional optical methods.
Welch can list a catalog of other innovative projects that are in progress. As part of the molecular imaging center that he established in 2002 with a five-year, $9.4 million National Cancer Institute (NCI) grant, David Piwnica-Worms, MD, PhD, is continuing to develop optical and other techniques to investigate cancers. Yuan-Chuan Tai, PhD, a physicist, is devising high-resolution devices for improving combined positron emission tomography (PET) and computed tomography (CT) scans. And through a new NCI grant, Victor Song, PhD, is working on novel magnetic resonance imaging (MRI) techniques for the diagnosis and staging of prostate cancer.
Imaging in clinical research
Beyond laboratory research, construction is progressing on a Center for Clinical Imaging Research (CCIR), due to open in 2007 on the tenth floor of Barnes-Jewish Hospital. The CCIR – the only one of its kind in the United States – will facilitate clinical research on hospital inpatients and offer easy access for outpatients. The center’s range of imaging equipment will be comprehensive: two MRI scanners, a PET/CT scanner, a CT scanner, an ultrasound imaging system and a regular PET scanner.
Most of these machines represent the latest equipment from Siemens Medical Systems, and the company will update the technology as improvements become available. The CT scanner, for example, will be the new Somatom Definition system, which offers extraordinary speed in collecting CT data and may eliminate the need for a contrast agent.
“The CCIR should greatly enhance the role of imaging in clinical research,” says Mark Mintun, MD, professor of radiology, who spearheaded the effort to create the CCIR. “Investigators at Siteman, including our young scientists, will have greater access to high-quality imaging systems, and it will be more convenient for patients to undergo imaging as part of their research studies.”
Siteman’s Imaging Response Assessment Team (IRAT) is designed to promote the use of effective imaging in clinical research, particularly as a way to assess patients’ response to therapy. The IRAT, one of eight formed nationally through NCI grants, integrates radiologists into the planning of clinical trials. In addition, it aims to make imaging as easy and efficient as possible, both for radiologists reading films and oncologists conducting research.
Under the direction of Barry Siegel, MD, chief of the division of nuclear medicine and IRAT leader, this effort already has changed the way imaging is conducted at Siteman. “We are using the IRAT as a resource to make certain that any clinical trials we plan here have the best imaging they possibly can,” Siegel says.
Cross-campus collaboration
Outside of the Department of Radiology, imaging researchers at Siteman are collaborating with chemist Karen Wooley, PhD, James S. McDonnell Distinguished University Professor in Arts and Sciences. Several years ago, Wooley joined with chemistry professor John-Stephen Taylor, PhD, and Welch to test a promising new concept: using nanoparticles – extremely small particles less than one-billionth of a meter in size – to image cancer. This kind of imaging could be used to check for a recurrence in cancer patients. Physicians would administer nanoparticles carrying recognition and radioactive elements, and those particles could be used in conjunction with PET scanning to highlight cancerous cells.
Wooley and her colleagues have been working since then to lay the scientific groundwork for this use of nanomaterials. “We are probing how these systems operate on a molecular level and then trying to optimize them,” she says.
In 2005, Wooley received a five-year, $12.5 million grant from the National Heart, Lung and Blood Institute to establish a Program of Excellence in Nanotechnology (PEN) – one of only four such programs in the country. She and a multidisciplinary team that includes 13 Washington University collaborators and two from outside the institution are working to advance this research.
“We are designing the nanoparticles to have specific chemistries, structures and properties and controlling those on a molecular level to try to understand differences in the way they interact with biology, including cancer cells,” Wooley says.
Research aims to affect patient care
An important frontier at the Siteman Cancer Center is the battle against brain cancer in adults and in children. In the field of neuro-oncology, the branch of medical science dealing with tumors of the brain and central nervous system, Siteman is poised to speed the development of innovative therapies thanks to its highly integrated, multidisciplinary team of researchers and clinicians.
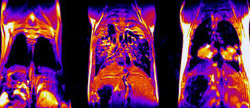
One of these team members is Joel Garbow, PhD, research associate professor of radiology, who works at the interface of chemistry, physics and biology. Garbow uses small-animal models to develop new magnetic resonance imaging (MRI) techniques that will ultimately help patients.
“Imaging plays a huge role, both in understanding the fundamentals on the research side and in the way we practice medicine,” Garbow says. “When we succeed in doing better research, the patients will do better, too.”
For the past four years, Garbow has been working with a team headed by David Gutmann, MD, PhD, Donald O. Schnuck Family Professor of Neurology, to better visualize tumors along the optic pathway in children who have neurofibromatosis type 1 (NF1), an inherited tumor predisposition syndrome. It is critically important to determine the extent of these tumors and limit unnecessary treatment in the brain.
Now, the team has developed an MRI method using a novel contrast agent that allows rapid, reliable and quantifiable identification of optic pathway tumors in NF1 mouse models developed by Gutmann. With this method, the researchers can quickly see the optic nerve and differentiate healthy tissue from tumor, laying the groundwork for important preclinical trials of potential drugs for the treatment of these tumors.
In another research project using advanced MRI techniques, Garbow and others are characterizing glioma, a highly aggressive form of brain cancer, to identify early, subtle signs that treatment is working. These experiments include efforts to measure such factors as changes in the tumor’s blood supply and permeability, the motion of water in the cells and cell density.
The team aspect of this effort is important, Garbow says. His own laboratory includes experts in physics, chemistry and various biological disciplines. On the NF1 team, adds Gutmann, are specialists not only in small-animal imaging but also in such areas as cell biology and signaling pathways. Clinicians always work with basic scientists to set the research agenda.
“Having this highly interactive, multidisciplinary team has allowed us to move more seamlessly from the research bench to the clinic,” Gutmann says. “If clinicians help drive the basic science questions, what comes out of the laboratory is more meaningful to the patient.”
In 2005, the Emerson Charitable Trust and the Anheuser-Busch Foundation provided funds through the Emerson/Anheuser-Busch Challenge to support Siteman’s work in neuro-oncology. The $10 million Challenge, which matches funds generated by Siteman, Washington University and Barnes-Jewish Hospital, is being used to advance research and patient care at the cancer center.
This story was featured in the 2006 Siteman Cancer Center annual report. Download a PDF file of the report.