Brain activity has been compared to a light bulb turning on in the head. Scientists at Washington University School of Medicine in St. Louis have reversed this notion, creating a drug that stops brain activity when a light shines on it.
The unexpected result, reported online in Nature Neuroscience, turned several lights on in researchers’ heads.
“This is daydreaming at this point, but we might one day combine this drug with a small implanted light to stop seizures,” says senior author Steven Mennerick, Ph.D. associate professor of psychiatry and of anatomy and neurobiology. “Some current experimental epilepsy treatments involve the implanting of an electrode, so why not a light?”
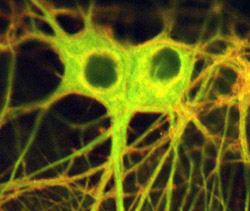
The new compound activates the same receptor used by many anesthetics and tranquilizers, making it harder for a brain cell to respond to stimulation. Mennerick and colleagues including lead author Larry Eisenman, M.D., Ph.D., assistant professor of neurology, tested the drug on cells in culture set up to behave like they were involved in a seizure, with the cells rapidly and repeatedly firing. When they added the new drug and shone a light on the cells, the seizure-like firing pattern calmed.
If the drug is adapted for epilepsy, Mennerick notes, it is most likely to help in cases where seizures consistently originate from the same brain region. Theoretically, doctors could keep a patient on regular doses of the new drug and implant a small fiber optic light in the dysfunctional region. The light would activate the drug only when seizure-like firing patterns started to appear.
Scientists in the laboratory of Douglas F. Covey, Ph.D., professor of molecular biology and pharmacology, created the drug by linking a steroid known to have anesthetic effects with a molecule, known as NBD, that fluoresces in response to blue light. Mennerick and colleagues were hoping to use the new compound, which they call the NBD-steroid, to trace the steroid’s path in the nervous system.
To their initial disappointment, the researchers found that adding the fluorescent tag to the steroid had disabled it.
“Normally, the steroid keeps the cell quiet in the face of stimuli that would otherwise cause it to fire,” Mennerick says. “That’s why drugs like barbiturates and Valium, which act on the same receptor as the steroid, are sedatives—they quiet the nerve system down.”
When dosed with NBD-steroid, nerve cells still responded to stimuli as readily as they had prior to exposure. Just to see where the modified steroid was going, though, researchers exposed the cells to light.
“All of a sudden, the response to the steroid was back, and the nerve cells were more reluctant to react to stimuli,” Mennerick says. “And we knew we had found something very interesting.”
To confirm what was happening, scientists dosed two of a nerve cell’s many different branches with NBD-steroid. When they shone a light on one of the branches, its readiness to respond decreased, while the readiness of the branch not exposed to light remained the same.
Department of Anesthesiology colleagues tested the compound’s effects on tadpoles.
“Tadpoles rapidly take up drugs through their skin, so they’re frequently used to test potential anesthetics,” Mennerick notes. “And of course, given that it’s a photoactive drug, they make a nice test subject because they’re mostly translucent.”
Tadpoles swimming in a solution of NBD-steroid went to sleep at the bottom of their beaker when exposed to light.
Mennerick and his colleagues are currently seeking to identify or create an animal model of epilepsy that lets them test the NBD-steroid’s potential as a therapeutic.
They are also looking for a new fluorescent tag that responds to longer wavelengths of light. Unlike many photoactive compounds, the NBD-steroid responds not to ultraviolet light but to light from the blue region of the electromagnetic spectrum. This helps because the longer wavelengths of blue light penetrate farther into tissue than ultraviolet light and are less damaging to it. Molecules that fluoresce in response to even longer wavelengths of light are available, and scientists are testing whether any of them can create the same effect when bound to the steroid.
Eisenman LN, Shu H-J, Akk G, Wang C, Manion BD, Kress GJ, Evers AS, Steinbach JH, Covey DF, Zorumski CF, Mennerick S. Anticonvulsant and anesthetic effects of a fluorescent neurosteroid analog activated by visible light. Nature Neuroscience, Feb. 25, 2007.
Funding from the Bantly Foundation and the National Institutes of Health supported this research.
Washington University School of Medicine’s full-time and volunteer faculty physicians also are the medical staff of Barnes-Jewish and St. Louis Children’s hospitals. The School of Medicine is one of the leading medical research, teaching and patient care institutions in the nation, currently ranked fourth in the nation by U.S. News & World Report. Through its affiliations with Barnes-Jewish and St. Louis Children’s hospitals, the School of Medicine is linked to BJC HealthCare.