“The heart is the single most energy-consuming organ per weight in the body,” says Lisa de las Fuentes, M.D.
Under some conditions this energy-hungry organ is prone to defects in its energy metabolism that contribute to heart disease, according to research published in a recent issue of the Journal of Nuclear Cardiology by de las Fuentes and colleagues at Washington University School of Medicine in St. Louis.
Earlier research led by de las Fuentes’ colleague Robert J. Gropler, M.D., showed that heart muscle in people with diabetes is overly dependent on fat for energy. Even though fat is an efficient fuel, burning it for energy creates an unusually high demand for oxygen, making the diabetic heart more sensitive to the drops in oxygen levels that occur with coronary artery blockage.
Gropler is director of the Cardiovascular Imaging Laboratory at the Mallinckrodt Institute of Radiology at the School of Medicine and professor of radiology, medicine and biomedical engineering.
Now this group of Washington University researchers has shown that hearts of non-diabetics with muscle thickening due to high blood pressure have an energy metabolism skewed in the opposite direction — away from the use of fat for energy.
“Whereas Dr. Gropler found that a high level of fatty acid metabolism could be detrimental, we show that a low level may also be harmful,” says de las Fuentes, co-director of the Cardiovascular Imaging and Clinical Research Core Laboratory and assistant professor of medicine. “These findings aren’t contradictory. The heart has to be able to choose the energy source, either fats or glucose, most appropriate for its current energy needs and the availability of fuel.”
De las Fuentes explains that hearts with muscle thickening, or hypertrophy, get less energy because of their reduced fat metabolism, which leads them to rely more heavily on carbohydrates.

“Carbohydrates produce less energy per molecule than fatty acids,” she says. “With hypertrophy, the heart has a higher energy demand because there’s more muscle to feed. With less fat metabolism, a greater reliance on carbohydrates may represent a shift to a less-efficient fuel.”
The metabolic abnormality can eventually lead to impaired contraction of the heart and to heart failure.
Animal studies by collaborators at Washington University have shown that in mice with thickened heart muscle, genes associated with transporting and breaking down fatty acids are less active than normal — in other words, the heart’s fat-burning machinery is malfunctioning.
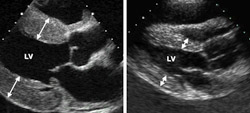
In this human study, the researchers studied patients who had high blood pressure that resulted in hypertrophy of the muscle of the left ventricle, the chamber of the heart that pumps blood to the body. The study showed that the greater the muscle mass of the hypertrophic heart, the lower the ability to burn fat. Magnetic resonance scans suggested that hypertrophic heart muscle had subtle abnormalities in contractile function at rest and was less energy efficient.
Normally heart muscle will alter between using fats and carbohydrates as fuel depending on availability. But at times of the day when blood glucose is low — such as when a person hasn’t eaten in a while — hypertrophic hearts can’t switch to burning fatty acids as normal hearts would, possibly leaving them energy deficient, de las Fuentes explains.
“This is the first time these data have been shown in humans,” says senior author Victor G. Dávila-Román, M.D., director of the Cardiovascular Imaging and Clinical Research Core Laboratory and professor of medicine, anesthesiology and radiology. “That is particularly significant because hypertension (high blood pressure) is a huge public health problem in the United States. Of the 65 million people with hypertension, between 25 and 50 percent of them have some evidence that their heart has been affected by high blood pressure.”
Not everyone who has high blood pressure will develop hypertrophy, and not everyone with hypertrophy has long-term problems, according to de las Fuentes. Some people appear to be protected while others appear to be at increased risk, likely due to genetic factors.
“Because we have this evidence that shows that fatty acid metabolism may play a role in this process, we are looking for variations in the metabolism genes in an ongoing clinical study,” de las Fuentes says.
Dávila-Román adds that by looking at the genetics of hypertension and hypertensive heart disease, they hope to identify genes that predispose people to both good and bad traits associated with these disorders. Such information promises opportunities for both prevention and treatment of cardiac disease.
de las Fuentes L, Soto PF, Cupps BP, Pasque MK, Herrero P, Gropler RJ, Waggoner AD, Dávila-Román VG. Hypertensive left ventricular hypertrophy is associated with abnormal myocardial fatty acid metabolism and myocardial efficiency. Journal of Nuclear Cardiology 2006; 13(3):369-77.
Funding from the National Institutes of Health, the Barnes-Jewish Hospital Foundation, the Robert Wood Johnson Foundation and the Sandra A. Daugherty Foundation supported this research.
Washington University School of Medicine’s full-time and volunteer faculty physicians also are the medical staff of Barnes-Jewish and St. Louis Children’s hospitals. The School of Medicine is one of the leading medical research, teaching and patient care institutions in the nation, currently ranked fourth in the nation by U.S. News & World Report. Through its affiliations with Barnes-Jewish and St. Louis Children’s hospitals, the School of Medicine is linked to BJC HealthCare.