On March 17, 2020, Pfizer Inc. and German-based BioNTech announced a collaborative effort to develop a vaccine for COVID-19, the disease caused by the SARS-CoV-2 virus.
Contributing to the global endeavor is Pfizer’s research and development (R&D) and process development facility in Chesterfield, Missouri — just a 20-minute drive from Washington University. It’s not a surprise then that several university alumni are contributing to the vaccine effort as well.
The WashU alumni working at Pfizer are diverse, including a recent graduate from Zimbabwe via Germany and an 18-year veteran of the company who started working at Pfizer the day after graduation. Yet they share similar intangible traits.
They are quick to smile, even when they talk about working until the sun rises.
They don’t miss a beat when it comes to acknowledging the importance of others, calling out by name their coworkers, past professors and advisers to spread the credit around.
And without saying it, they are proud — proud of themselves, their company and their alma mater.
‘No, no, look at these numbers!’
In the midst of a viral pandemic, who would you want to work on vaccine development and safety?
A graduate of Washington University in St. Louis, naturally.
And probably someone with a background in some medical research. Even better? Someone who had studied viruses.

It would be great if this person saw their job as aligning with their worldview — someone who wanted to help people and thought their work could help them do that.
And, since this is just a wish list, what if this person also liked to plot cases of a novel virus halfway across the world — you know, just for fun?
In the final weeks of December 2019, Aparna Deora, PhD ’00, noticed a WashU grad school friend of hers started posting about some virus in China. These postings carried special interest for several reasons, including Deora and her family had scheduled a 2020 spring break trip to China.
“I started plotting out the numbers in China,” she says, “and I thought, ‘This is bad! This is growing exponentially.’” Deora’s husband said not to worry, their trip wouldn’t be affected.
“I said, ‘No, no, look at these numbers!’”
Deora’s trip was canceled, which was good news, not just for her and her family’s health, but in a very real way, for all of us. She is one of the many WashU alumni who have had a hand in developing, testing and manufacturing BNT162b2, the first vaccine to be granted emergency use authorization for COVID-19.
Deora has been at Pfizer since finishing her postdoctoral studies. “I’m a molecular virologist by training,” she says. “It’s somewhat eerie because I’ve always been big into books about pandemics and viral outbreaks. They’ve always fascinated me because of how quickly they move and their ability to evolve.”
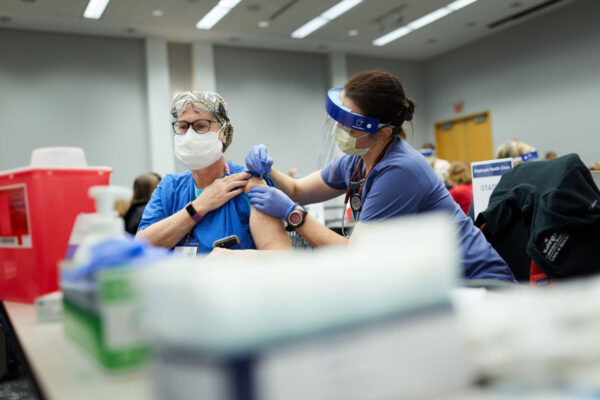
For three years, Deora has worked as the senior director of quality control, stability and microbiology at Pfizer; in a few months, she’ll transition to a new role as the vaccine category lead.
Since March 2020, however, she has been focused solely on the quality of one vaccine. Her team tests the product at all stages, including the raw materials that are manufactured in Chesterfield; the vaccine mRNA drug substance that is manufactured in Andover, Massachusetts; and the final drug product, vialed in Kalamazoo, Michigan, and Puurs, Belgium: “The vials that are about to be released to the public,” she says.
Deora’s casual interest in plotting cases of the virus gave her an early insight to the potential danger of SARS-CoV-2. But it wasn’t until late March that she understood the role she and her peers would play when it came to stopping this pandemic.
When she learned they would be partnering with BioNTech, a German-based biotechnology company, to develop a vaccine, “Suddenly I knew, Pfizer’s going to go there. That’s when I realized how different this was going to be.
“People laugh at me because I love my job so much. But I get to work on things that are in the clinic, helping people. I feel like my job is about hope.”
Aparna Deora, PHD ’00
“I love working for Pfizer,” Deora says. “People laugh at me because I love my job so much. But I get to work on things that are in the clinic, helping people. I feel like my job is about hope.”
She understood that her employer shared the same worldview when she saw the mobilization from the highest level in order to develop a COVID-19 vaccine. “If we needed a lot of people, the response was, ‘Go ahead, do it.’” If it was going to cost a lot of money, she says, the answer was always, “‘It doesn’t matter, go ahead and do it.’”
Deora says her career path wasn’t a given. She thought she might be a doctor, but after attending a women-in-science program at the University of Michigan, “I was like, this is what I love. I love the lab.”
At the Washington University School of Medicine, she worked in the lab of Lee Ratner, MD, PhD, a professor of medicine in the oncology division. Deora’s doctoral research didn’t necessarily foretell a career in the world of vaccines, however.
“To me, though, it’s just about good science,” she says, “and it’s something I’m passionate about.”
Her passion matches the gravity of today’s situation, which, she notes, is not simply that we are facing a new virus, or even a pandemic.
“Throughout history we’ve faced pandemics; it’s happened before,” she says. “What’s unique today is the mobility you see in populations and the rapidity with which this virus can spread. It’s incredibly difficult to try to contain something under these conditions.”
To her point, although she knew it would be bad, “I didn’t think it would be this,” she says, via Zoom, looking behind her. “In my wildest dreams, I didn’t think I’d be talking to you from my upstairs bedroom.”
Process science: Kind of like cooking
One of the first projects Tatenda Shopera, MSChE ’16, PhD ’18, worked on as a PhD student at the McKelvey School of Engineering was with Tae Seok Moon, associate professor of energy, environmental and chemical engineering. Shopera remembers the day Moon selected him to join the lab. “He believed in me from day one,” Shopera says. “I consider myself very fortunate to have had him as my adviser.”
The engineering school project, funded by the Bill and Melinda Gates Foundation, was aimed at ending the transmission of dangerous parasites in developing countries.

“I’ve always been drawn to these kinds of projects,” Shopera says of his desire to help others. “This was a motivating factor in going to work at Pfizer.”
Since March 2020 when Pfizer and German-based BioNTech announced plans to jointly develop a COVID-19 vaccine, Shopera says the pace has been fast, the challenges dynamic, and the work — to put it mildly — rewarding.
“I wanted to develop medicines and vaccines. I thought being at Pfizer might give me that opportunity,” he says.
He very quickly got the opportunity he sought.
Shopera went to work as a senior scientist at Pfizer in June 2019. The first case of the novel coronavirus was reported six months later. Three months after that, he was pulled into a COVID project.
As a process scientist, he worked to fine-tune the conditions in the environment to ensure the quality and consistency of the final product, a medicine or a vaccine.
“Think of it as cooking,” he says. At home, you have a recipe, but you also taste as you cook. You know you need a certain amount of, for instance, salt, he says. “But you want it to be tasty, so you have an idea that this is too much salt, or not enough water. In this way, you are manufacturing food and testing to assure quality.”
Shopera says his work is analogous, but instead of cooking for friends and family, when he first joined Pfizer, he was feeding cell cultures to develop manufacturing processes at laboratory scale. “We monitor and ask what do these cells like? What is it they do not like?” It’s not just a matter of keeping the cells happy. “If they don’t like the recipe, or the conditions are unsuitable, they are not going to give you what you are looking for.”
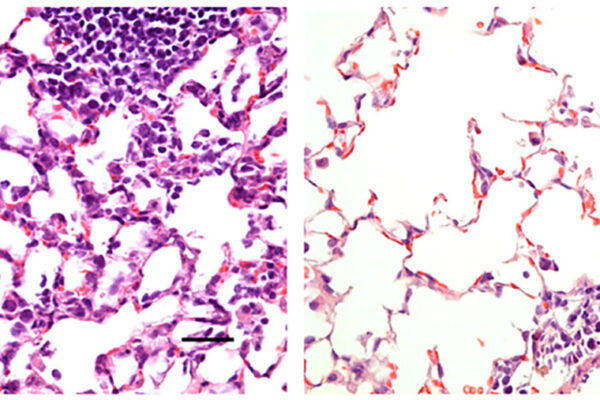
When he moved to the COVID-19 project, Shopera’s process development experience with cell cultures was put to use for another platform technology: mRNA, the so-called software that translates the instructions in our DNA into action in our cells. The correct recipe in his development lab yields a plasmid DNA encoded with a bit of mRNA that has instructions for making an antigen for SARS-CoV-2, the virus responsible for COVID-19.
“Now fast forward years later, I’m part of the team that is developing the vaccine and medicines.”
Tatenda Shopera, MSChE ’16, PhD ’18
This is the basis for the vaccine, which bypasses our DNA and directly tells our own cells to produce the antigen that stimulates our immune system, preparing it for an encounter with the real thing.
For Shopera, not only has he helped to make a life-saving vaccine, he is also living out the answer to a question he’s had for many years.
“I grew up in Zimbabwe. For the most part, we import medicines,” he says. “I always had that question: Where do medicines come from? Where do vaccines come from? Who comes up with the idea?” he says.
“Now fast forward years later, I’m part of the team that is developing the vaccine and medicines.”
You can’t always take the corporate jet, but sometimes, you can
Leading Shopera’s team is Rodney Combs, MA ’92, who studied biotechnology at WashU. Combs helps lead teams who were responsible for developing and scaling up the mRNA and pDNA manufacturing processes. Pfizer’s Chesterfield site is also responsible for manufacturing the plasmid DNA template — the entire world’s supply for the COVID-19 vaccine.

A week before Christmas in 2019, Combs was in New York meeting with colleagues from BioNTech and Pfizer’s Vaccine Research Unit to discuss mRNA vaccine technology. Combs had been leading an influenza research team. Because of their almost-modular nature, mRNA vaccines have the potential to be especially helpful responding to seasonal flu variations.
“Even in that moment,” Combs says, “I was thinking, ‘This is going to be great technology to quickly respond if there’s ever a pandemic.’’’ By March 2020, he says, he knew his life was going to change.
“It was a once-in-a-lifetime experience to know what you’re doing is going to be so critical for humankind,” he says. “Everyone understood, ‘I couldn’t be doing anything more important.’”
So he and his colleagues worked at an incredible pace, and soon the impossible seemed mandatory. They would joke: “Let’s write a license application in one week.” These applications typically take nine months or so. “We’d laugh at the first thought of an impossibility like this … then the video conference would get quiet,” he says. “And then? We’d do it.”
They were able to pull off this “billion-dollar bet,” as Pfizer’s endeavor has been referred to in the media, for a few reasons. They were able to pull a variety of people into the project with the required skill sets; they had the full backing of the company; and they were able to do things typically done sequentially in parallel.
“There were lots of risks,” he says. “You don’t know if the activity that takes six weeks is going to be successful, while, at the same time, you’re going ahead with an activity that takes three weeks,” but which is dependent on the success of the six-week activity.
“It’s amazing to think about how fast we did this,” he says. He credits the “incredible” team in Chesterfield — making sure to laud Shopera by name — as well as Pfizer’s determination to get this done.
He recalls a stumbling block they faced with shipping. There weren’t international commercial flights available to quickly send plasmid DNA to manufacturing sites in Europe to meet our aggressive timelines.
“So we used our corporate jet to fly packages from here to Mainz, Germany,” he says with a laugh.
Of course, you can’t send the corporate jet every time, but still, Combs says the team will likely carry over some lessons learned.
“It’s something we can be proud of, that so many WashU alumni are working on this, here in Missouri.”
Rodney Combs
“We don’t have the ability to do these things every time,” he says of pulling all-nighters or plucking people from other projects to join your team. But in the case of a true pandemic or an unmet medical need, you have the ability to sustain this level of dedication, he says.
“It’s something we can be proud of, that so many WashU alumni are working on this, here in Missouri.”
There will be more to be proud of in the future. Comb says these past months have taught them a lot about mRNA, as well as ways to streamline their operations. And just as he saw the potential for mRNA vaccines in the time of a pandemic, he’s again looking to the next big challenge. “If we can get this to work for the flu, that’s when you start thinking…,” he says. “This technology has given us a really big hope.”
Testing … everything
Understanding the ideal vaccine for seasonal flu helps to understand how it is that the COVID-19 vaccine seems — to the layperson, at least — as if it was developed in an absurdly short amount of time.
“People have been working on mRNA vaccines for several years. Whole companies have been established around the potential technology for decades,” says Justin Sperry, senior director of analytical research and development at Pfizer. “It’s designed to go fast. When you’re thinking about making a flu vaccine, you want to be able to increase the accuracy to match what strain is going around.”
Sperry, MA ’05, PhD ’08, whose chemistry adviser was Michael L. Gross, found out about COVID-19 like most of us: on the news in late December 2019. In late January 2020, he attended a conference with an assortment of industry scientists and health authority agencies, and he recalls chatter about whether or not the virus would make its way stateside.
Two weeks later, there were cases in Washington state and Boston. “By March, we were told Pfizer was going to start work on a vaccine,” he says. “It was all-hands-on-deck.”
Sperry leads a team responsible for developing the testing strategies, to ensure everything is running smoothly and the final product is consistent and meets strict specifications.
When pressed about what exactly he’s testing — Hardware? Processes? Efficiency? The final product? — he pauses.
It is … a long pause.
His one-word response belies the nature of the work: “Everything.”
That includes testing raw materials for the enzymatic reactions and the plasmid DNA. It means testing each step of the process, “to make sure it’s under control and runs exactly the same as last time,” he says. And, of course, it means evaluating the quality attributes of each major step, the DNA plasmid from the Chesterfield facility, the mRNA from Andover, Mass., and the final vaccine drug product, which is manufactured and finished in Kalamazoo, Mich. Every test must pass in order to release the batch.
Sperry and his team are also responsible for collecting and summarizing all of the results, which they submit to regulatory agencies, both in the United States and abroad.
“It takes a tremendous number of hours,” he says. “It’s a pretty exciting — and stressful — time.”
He hesitated when asked if he’d ever done anything like this before. On the one hand, he says, “Our teams are very familiar with vaccine development. That’s what we do. And we had been working on an mRNA vaccine for a couple of years.”
But in terms of the sheer speed of development? No. Like his coworkers, Sperry credits Pfizer for the zeal with which they took on the challenge. The gist of the company’s attitude was, “We must work on this. Resources are not an excuse. Here’s an open checkbook. Put as many people on it as you can to get it done with quality, integrity and speed.”
“We had to re-prioritize nearly every activity in the portfolio.”
Justin Sperry, MA ’05, PhD ’08
And that’s what they did.
Of course, the scientists at Pfizer had been working on many other projects, working to eradicate other diseases. “We’re working on cancer therapies and rare diseases,” Sperry says. “We had to re-prioritize nearly every activity in the portfolio. Ultimately, we could not drop those projects, and had to squeeze in this gigantic one.”
It was less finesse and more brute force. When people were asked, “Who wants to work on the COVID vaccine?” every hand went up. People were willing to work extra hours, nights and weekends to deliver on their primary projects as well as this vaccine. “It was an amazing and proud feeling. That’s when you know this is a priority for everyone.”
“It’s fun and challenging, but it’s taken a lot of grit.”
Still work to be done
There have been days, Combs says, “I didn’t realize night was turning into morning. I was still sitting up, talking with my German colleagues.” But there’s no trace of weariness in his voice.
“It’s been a great opportunity to debut this technology,” he says. “And the spirit we had and resources that were made available … We were told to do whatever we can, to take down barriers. Anything we thought would slow us down was just put aside.”

“I work hard, I stay late, but I know I’m appreciated,” Deora says. “I’ll hear, ‘Wow, you stayed late last night, thank you.’”
And she and her colleagues will continue to stay late. Although the vaccine has thus far been a success, there is still work to be done.
“Everything has to be perfect from now until everyone is dosed,” Sperry says.
When asked when they’ll be able to sit back, kick up their feet and say: Well, we did it team. It’s over. Job well done! No one has a straight answer other than: When there are no more deaths from COVID-19.
“Yes, we’ve had victories along the way,” Shopera says. “And we do celebrate. If we can hit a milestone, we take a few seconds to celebrate. Then, we go back to work.
“Because right now, we are still living in the world of COVID-19.”