The fatigue and lack of motivation that many cancer patients experience near the end of life have been seen as the unavoidable consequences of their declining physical health and extreme weight loss. But new research from Washington University School of Medicine in St. Louis challenges that long-held assumption, showing instead that these behavioral changes stem from specific inflammation-sensing neurons in the brain.
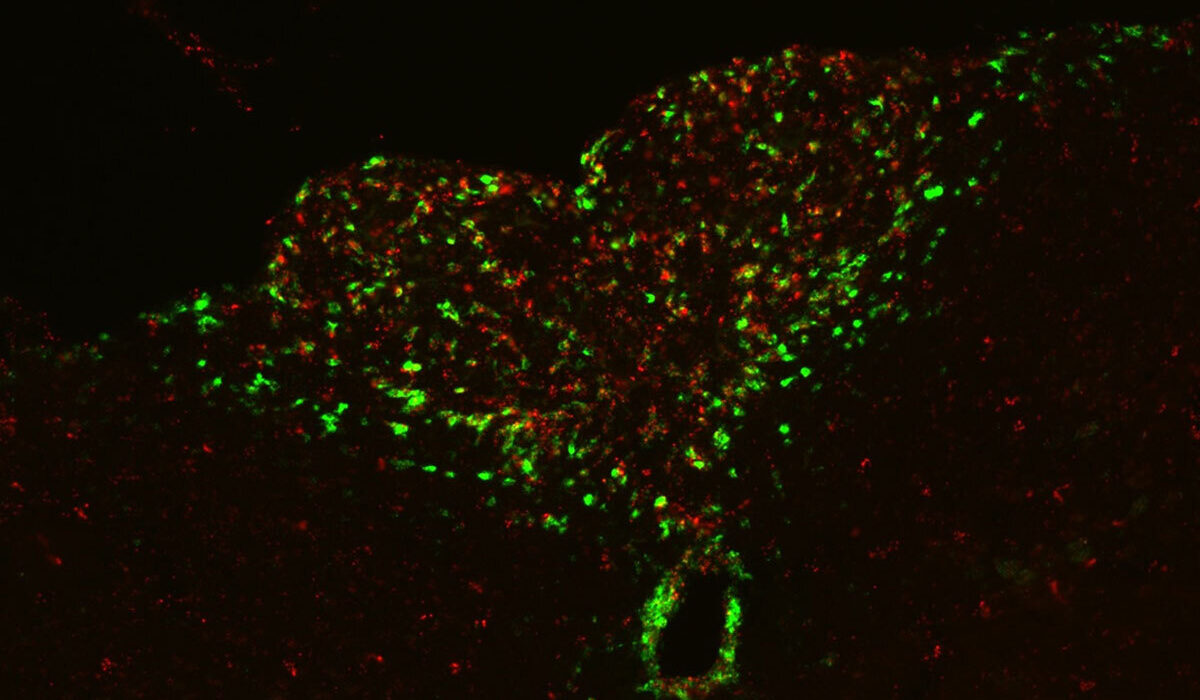
In a study published April 11 in Science, the researchers report that they identified a direct connection between cancer-related inflammation and the loss of motivation characteristic of advanced cancer. Studying mice with cancer-linked cachexia, a condition typical of the disease that leads to muscle wasting and weight loss, they discovered a previously unrecognized pathway in the brain. This pathway senses inflammation and actively suppresses dopamine — a key driver of motivation — resulting in apathy and loss of drive.
Blocking the pathway restored motivation, even though the cancer and weight loss continued. This indicates that apathy can be treated separately from the disease itself.
“The implications of the research are profound,” said the study’s lead author, Adam Kepecs, PhD, a professor of neuroscience and of psychiatry at WashU Medicine. “We’ve uncovered a direct brain mechanism through which inflammation drives apathy in cancer, and we were able to restore normal motivation in mice with cachexia, despite ongoing inflammation as cancer progressed.”
About 70% of patients with advanced cancer experience cachexia. In addition to physical decline, patients often suffer from severe fatigue, apathy and a lack of motivation that affect their overall quality of life.
To understand whether these psychological symptoms are side effects that emerge from physical deterioration or whether they arise from distinct biological mechanisms, the research team, including Marco Pignatelli, MD, an assistant professor of psychiatry at WashU Medicine, and Tobias Janowitz, MD, PhD, an associate professor at Cold Spring Harbor Laboratory, turned to a well-validated mouse model of cancer cachexia. They focused specifically on behavioral symptoms, which had not previously been investigated, and mapped the brain regions involved.
They discovered that a structure in the brainstem, a part of the brain that controls vital functions such as breathing and heart rate, acts as a sensor for inflammatory signals in the bloodstream, particularly a molecule called interleukin-6 (IL-6), which is elevated in cancer cachexia. When IL-6 levels rise, neurons in this region of the brainstem transmit a signal through a defined pathway that suppresses dopamine release in a part of the brain called the nucleus accumbens, which is key for motivation and reward. The resulting drop in dopamine had the effect of making the mice less motivated to exert themselves to complete activities.
To see if interfering with this response could treat the lack of motivation and apathy, Kepecs and his colleagues tried two different approaches: they boosted dopamine levels and blocked inflammation-sensing neurons in the brainstem. Both approaches eliminated or reduced apathy in the mice. Treating the mice with an IL-6 antibody similar to an existing FDA-approved drug for rheumatoid arthritis, an inflammatory condition, also restored the animal’s motivation, a finding that points to a potential treatment for the psychological symptoms associated with advanced cancer.
“What’s remarkable is that motivation was restored even in late-stage disease,” said Pignatelli. “It suggests we may be able to improve quality of life by targeting the brain circuit.”
For acute illnesses such as infections, this inflammation-driven reduction in motivation may be adaptive, helping the body conserve energy to fight off disease, Kepecs explained. But in chronic conditions such as cachexia, prolonged apathy — including a reduced drive to eat, move or engage socially — can become harmful, worsening health and quality of life. Because IL-6 — the inflammatory molecule driving this effect — is elevated in many other conditions, and the brain regions involved are central to motivation, this same circuit likely contributes to apathy across a range of chronic illnesses.
“This gives us a new way to understand apathy in advanced cancer,” said Kepecs. “It’s not just a byproduct of physical decline, but a direct response to inflammation in the brain. That means we can potentially target the underlying biology to improve motivation and quality of life — even when the cancer itself is no longer treatable.”
Zhu XA, Starosta S, Ferrer M, Hou J, Chevy Q, Lucantonio F, Muñoz-Castañeda R, Zhang F, Zang K, Zhao X, Fiocchi FR, Bergstrom M, Siebels AA, Upin T, Wulf M, Evans S, Kravitz AV, Osten P, Janowitz T, Pignatelli M, Kepecs A. A neuroimmune circuit mediates cancer cachexia-associated apathy. Science. April 11, 2025. DOI: 10.1126/science.adm8857
This research was funded by the National Institute of Child Health and Human Development of the National Institutes of Health (NIH) grant P50 HD103525, Deutsche Forschungsgemeinschaft grant DFG -STA 1544, LaCaixa, the Mark Foundation for Cancer Research grant 20-028-EDV, the Simons Foundation, Cancer Grand Challenges, NIH grant 1OT2CA278690-01, CRUK: CGCATF-2021/ 100019, and NIH/National Cancer Institute grant R37CA286477-01A1, Cancer Center Support grant 5P30CA045508, NIMH grant MH130610, the Taylor Family Institute for Innovative Psychiatric Research, the Hope Center Pilot Grant, the McDonnell Center for Systems Neuroscience Small Grant, and the NARSAD Young Investigator Grant 27102 and P&S Fund, a WUSTL BJC investigator award and NIH grant DP1 MH14002. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
About Washington University School of Medicine
WashU Medicine is a global leader in academic medicine, including biomedical research, patient care and educational programs with 2,900 faculty. Its National Institutes of Health (NIH) research funding portfolio is the second largest among U.S. medical schools and has grown 56% in the last seven years. Together with institutional investment, WashU Medicine commits well over $1 billion annually to basic and clinical research innovation and training. Its faculty practice is consistently within the top five in the country, with more than 1,900 faculty physicians practicing at 130 locations and who are also the medical staffs of Barnes-Jewish and St. Louis Children’s hospitals of BJC HealthCare. WashU Medicine has a storied history in MD/PhD training, recently dedicated $100 million to scholarships and curriculum renewal for its medical students, and is home to top-notch training programs in every medical subspecialty as well as physical therapy, occupational therapy, and audiology and communications sciences.
Originally published on the WashU Medicine website