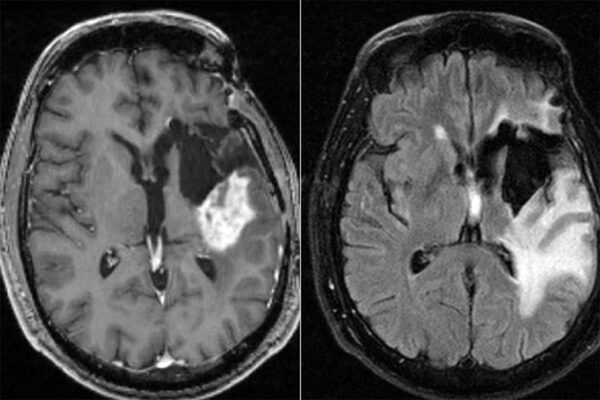
Glioblastoma is an aggressive brain cancer that has no cure. A recent chart study of patients with glioblastoma found that taking chemotherapy in the morning was associated with a three- to six-month increase in median survival.
Now a study from Washington University in St. Louis reports that glioblastoma cells have built-in circadian rhythms that create better times of day for treatment.

Biologists and clinicians recorded daily rhythms in “clock gene” expression from a variety of cultured human and mouse glioblastoma cell lines and isolates. These rhythms aligned with daily activity of a DNA repair enzyme known as MGMT. The scientists then conducted tests and found that tumor cells were more likely to die when chemotherapy was administered at the time of day — the morning — when tumor cells had the least MGMT activity.
Repeating their efforts in mice with glioblastoma, the scientists found that morning administration of chemotherapy decreased tumor size and increased body weight compared with evening drug delivery.
The study was published in the Journal of Neuro-Oncology.
“There might be an avenue for better treating this disease with a drug at the times of day when the cells are more susceptible,” said Maria F. Gonzalez-Aponte, a graduate student in biology in Arts & Sciences at Washington University, who is a first author of the new study. “We found that delivering chemotherapy with temozolomide (TMZ) in the subjective morning can significantly decrease tumor growth and improve disease outcomes for human and mouse models of glioblastoma.”

“Because TMZ is taken orally at home, translation of these findings to patients is relatively simple,” said Erik D. Herzog, PhD, the Viktor Hamburger Distinguished Professor and a professor of biology in Arts & Sciences, corresponding author of the new study.
“We will need additional clinical trials to verify our laboratory findings, but evidence so far suggests that the standard-of-care treatment for glioblastoma could be improved simply by asking patients to take the approved drug in the morning,” Herzog said.
While largely understudied for TMZ and glioblastoma, the practice of considering time of day in treating disease has been shown to improve outcomes in several cancers, including acute lymphoblastic leukemia, colorectal and ovarian and other gynecological cancers, study authors noted. Joshua B. Rubin, MD, PhD, a professor of pediatrics and of neuroscience at the School of Medicine, is a longtime collaborator with the Herzog laboratory and a co-author on the paper. Gary J. Patti, PhD, a professor of chemistry in Arts & Sciences and of medicine at the School of Medicine, and staff scientist Kevin Cho, PhD, in chemistry are also co-authors.
Findings from this study have implications for both treatment and diagnosis of glioblastoma.
In general, glioblastoma patients who are diagnosed with what is called MGMT methylated tumors tend to respond better to chemotherapy with TMZ.
But this study found that MGMT methylation levels rise and fall based on the circadian time of the tumor. As a result, doctors should control for the time of day when the biopsy of a tumor is taken to properly compare results and improve diagnoses, study authors said.
“Despite extensive research over the past 20 years, the median survival for glioblastoma patients post-treatment remains at about 15 months, a grim statistic,” Herzog said. “Incorporating chronotherapy, or timed delivery of drugs, could help improve things.”
Herzog, Patti and Rubin are research members of Siteman Cancer Center at Barnes-Jewish Hospital and Washington University School of Medicine.
Funding: This work was supported by National Institutes of Health (NIH) grants NINDS R21NS120003 and the Washington University Siteman Cancer Center. This content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Gonzalez-Aponte, M.F., Damato, A.R., Trebucq, L.L. et al. Circadian regulation of MGMT expression and promoter methylation underlies daily rhythms in TMZ sensitivity in glioblastoma. J Neurooncol (2024). https://doi.org/10.1007/s11060-023-04535-9