Cardiologists and radiation oncologists at Washington University School of Medicine in St. Louis pioneered the use of radiation therapy — a strategy typically used against cancer — to treat patients with a life-threatening abnormal heart rhythm called ventricular tachycardia.
Now, after studying the cardiac effects of radiation in a small number of these patients and modeling the effects of low-dose radiation in mice with heart failure, the research team has found that low-dose radiation therapy appears to improve heart function in various forms of heart failure. More research is needed before the investigators can evaluate this therapy in patients with heart failure, but the study suggests that radiation’s effects on injured hearts with high levels of inflammation may be more varied — and perhaps beneficial — than previously understood.
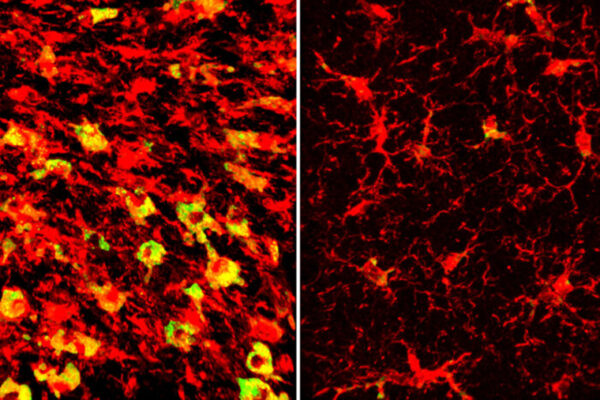
The study, published Nov. 28 in the journal Med, suggests that low-dose radiation therapy improves heart function, at least in part, by reducing the number of inflammatory immune cells in the heart muscle.
“The radiation therapy used to treat ventricular tachycardia is targeted to a specific location in the heart; however, a large portion of the rest of the heart gets a low-dose exposure,” said co-senior author and cardiologist Ali Javaheri, MD, PhD, an assistant professor of medicine. “We wanted to understand the effects of that low-dose radiation on these patients’ hearts. There was concern that it could be harmful to overall heart function, even though it treats dangerous arrhythmia. We were surprised to find the opposite: Heart function appeared to be improved after radiation therapy, at least in the short term.”
About 6.2 million American adults currently live with heart failure, according to the Centers for Disease Control and Prevention. More than half of heart failure patients hospitalized for the condition die within five years of that first hospitalization, demonstrating a need for better therapies. A failing heart gradually loses its ability to properly supply the body with oxygenated blood. A complex condition, heart failure can have diverse triggers, including a past heart attack, viral infection or chronic arrhythmias such as ventricular tachycardia.
A group of nine patients with ventricular tachycardia was evaluated with cardiac MRI before and after radiation treatment, with the MRIs showing improved heart function soon after radiation. In particular, the patients’ hearts showed improved pumping capacity of the left ventricle, which supplies blood to the entire body. The improvement was seen a few days after treatment, so it was deemed unlikely to be due to the reduction of the arrhythmia, which happens more gradually over the ensuing weeks and months.
The researchers also studied the effects of similar low-dose radiation to the heart in groups of mice with heart failure from three different causes. Similar to what was observed in the human patients, the researchers found improved heart function in mice receiving radiation therapy, especially in the left ventricle. In the mice with progressive heart failure, radiation therapy increased survival of the animals, indicating that improvements in heart function translated to improved survival.
The researchers found that the failing mouse hearts that received radiation had reduced fibrosis — or scar tissue — and reductions in cardiac macrophages, a type of immune cell that can drive inflammation in the heart. In general, the irradiated hearts had fewer cells that proliferate quickly — such as immune cells and fibroblasts — which tend to contribute to worsening heart failure. In contrast, normal heart muscle cells generally do not divide often, if at all.
“We know that rapidly dividing cells — such as cancer cells, for example — tend to be more susceptible to death by radiation,” said co-senior author and radiation oncologist Carmen Bergom, MD, PhD, an associate professor of radiation oncology. “The effect we see in these hearts is likely more complex than a simple reduction of rapidly dividing inflammatory immune cells. We are continuing our research to delve more deeply into what else may be happening, but we have been pleasantly surprised to see evidence that low-dose radiation in these hearts may reduce inflammation and help remodel the heart in a way that is beneficial.”
To understand more about radiation’s effects on the heart, the researchers plan to continue their investigations of the patients already receiving radiation therapy for ventricular tachycardia. The current study showed, via MRI, improved heart function. Next, the researchers plan to conduct more advanced studies to see if there is evidence of reduced inflammation in the human hearts, similar to what they found in mice.
Pedersen LN, Valenzuela Ripoll C, Ozcan M, Guo Z, Lotfinashsh A, Zhang S, Ng S, Weinheimer C, Nigro J, Kovacs A, Diab A, Klass A, Gorgan F, Cho Y, Ataran A, Luehmann H, Heck A, Kolb K, Strong L, Navara R, Walls GM, Hugo G, Samson P, Cooper D, Reynoso FJ, Schwarz JK, Moore K, Lavine K, Rentschler SL, Liu Y, Woodard PK, Robinson C, Cuculich PS, Bergom C, Javaheri A. Cardiac radiation improves ventricular function in mice and humans with cardiomyopathy. Med. Nov. 28, 2023.
This work was supported by the National Institutes of Health (NIH), grant numbers K08HL138262, 1R01HL155344, P30DK020579, P30DK056341, R01HL147884, R01HL163274, 5R35HL145212, 5P41EB025815, P30DK052574, S10 OD028597 and S10 OD020136-01; the Children’s Discovery Institute of Washington University and St. Louis Children’s Hospital, grant number MC-FR-2020-919; an American Heart Association Postdoctoral Fellowship, grant number 898679; the American Heart Association Collaborative Sciences Award, number 19CSLOI34630021; a Fulbright Scholarship (SCH-PS00352868-2023-1); a Cancer Research UK Postdoctoral Bursary (RCCPOB-Nov22/100010); a T32 fellowship (T32CA113275) and ASTRO Residents/Fellows Seed Grant (P23-04623); and the Burroughs Wellcome Career Award for Medical Scientists. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
About Washington University School of Medicine
WashU Medicine is a global leader in academic medicine, including biomedical research, patient care and educational programs with 2,800 faculty. Its National Institutes of Health (NIH) research funding portfolio is the third largest among U.S. medical schools, has grown 52% in the last six years, and, together with institutional investment, WashU Medicine commits well over $1 billion annually to basic and clinical research innovation and training. Its faculty practice is consistently within the top five in the country, with more than 1,800 faculty physicians practicing at 65 locations and who are also the medical staffs of Barnes-Jewish and St. Louis Children’s hospitals of BJC HealthCare. WashU Medicine has a storied history in MD/PhD training, recently dedicated $100 million to scholarships and curriculum renewal for its medical students, and is home to top-notch training programs in every medical subspecialty as well as physical therapy, occupational therapy, and audiology and communications sciences.