Researchers at Washington University School of Medicine in St. Louis have received a $6 million grant from the National Heart, Lung, and Blood Institute of the National Institutes of Health (NIH) to harness new understandings of the immune system to develop innovative therapies for heart failure and the prevention of organ rejection following heart transplantation.
The research will build on work led by principal investigator and cardiologist Kory J. Lavine, MD, PhD, an associate professor of medicine. Lavine and his team have identified important immune cells in the heart, called macrophages, that play key yet diverging roles in damaging inflammation and beneficial healing. Whether specific macrophages are helpful or harmful depends on where in the body the cells originate. Macrophages involved in healing develop and reside within the heart, while the harmful macrophages are recruited from the bone marrow during times of stress and injury. Finding ways to block the harmful cells from the bone marrow and nurture the healing ones already in the heart could lead to new therapies for various types of heart failure and methods to protect a transplanted heart from being rejected by the body’s immune system.
“We are excited about research in cardiovascular medicine that could open the door to reducing inflammation and promoting healing in the failing heart,” Lavine said. “This program grant will help us pursue the development of therapeutics and ways of treating heart failure that were not possible before.”
Lavine’s lab recently published several studies highlighting the major research themes the grant will continue to support.
In one study, Lavine and his colleagues showed that a protein called CCL17 makes heart damage worse by suppressing the action of specialized immune cells called regulatory T cells. Such cells reduce inflammatory responses when the heart is damaged. The study, published in the journal Circulation, suggests that inhibiting CCL17 could help resolve heart inflammation after the heart is injured by a heart attack, for example, and ultimately improve the organ’s recovery. Lavine is working with industry collaborators to develop antibodies that bind to and neutralize CCL17 to reduce its pro-inflammatory actions.
“If you can resolve inflammation earlier, you may be able to facilitate healing of the heart muscle, which will improve longevity and function after a heart attack,” said Lavine, also director of the Cardiovascular Precision Medicine Research Initiative in the Cardiovascular Division. “The hope is that blocking inflammation earlier can reduce fibrosis — the formation of scar tissue — and improve cardiac function long term.”
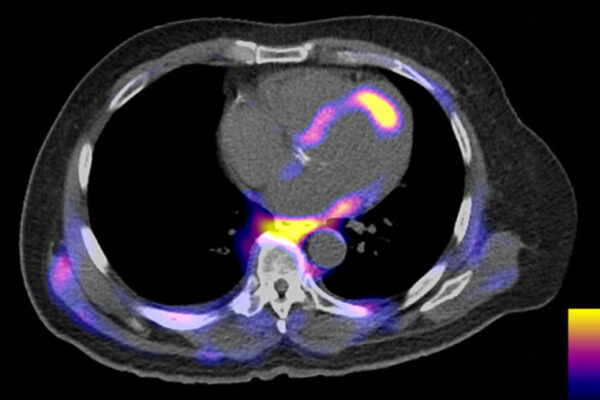
A second study, published in the journal Nature Cardiovascular Research, utilizes the latest single cell technologies to create the first comprehensive cellular atlas of human heart failure. Lavine and his team sequenced the hearts of 27 healthy donors and the hearts of 18 patients with dilated cardiomyopathy, a form of heart failure characterized by a thinning and weakening of the heart muscle. The atlas serves as an important new resource for researchers trying to understand and develop better therapies for heart failure.
A third study, in the journal Development, demonstrated that the researchers could utilize human pluripotent stem cells to create macrophages that recapitulate those originating in different parts of the body and that have divergent effects on the heart. Lavine and his team hope to leverage this new system to engineer macrophage populations that heighten capacity to help repair or rejuvenate the heart.
“A number of groups have shown in animal models that heart muscle cells derived from stem cells can be grafted onto the heart,” Lavine said. “There is the potential for this to be therapeutic, but these cells don’t integrate well into the surrounding tissue and tend to cause arrhythmias. A key property of reparative macrophages is their ability to help cells within tissues integrate — they can help connect cells electrically, which could possibly overcome the current barriers standing in the way of stem cell-based therapies to repair or even regenerate portions of the human heart.”
Similar to the way immune-based therapies have revolutionized the treatment of a number of cancers, this grant may be a step toward harnessing knowledge of the immune system to reduce cardiovascular inflammation and maximize the regenerative potential of the human heart.
Washington University School of Medicine’s 1,700 faculty physicians also are the medical staff of Barnes-Jewish and St. Louis Children’s hospitals. The School of Medicine is a leader in medical research, teaching and patient care, and currently is No. 4 in research funding from the National Institutes of Health (NIH). Through its affiliations with Barnes-Jewish and St. Louis Children’s hospitals, the School of Medicine is linked to BJC HealthCare.