A new study led by researchers at Washington University School of Medicine in St. Louis suggests that a widely used heart failure drug named sacubitril/valsartan is no better than valsartan alone in patients with severe heart failure. The study also provides evidence that the treatment with valsartan may be slightly safer for patients with advanced heart failure.
The study was published online Nov. 3 in JAMA Cardiology.
Heart failure is one of the leading causes of hospitalization in the United States, with about two heart failure hospitalizations occurring every minute. It is often triggered by damage to the heart from, for example, a heart attack or a viral infection. A complex clinical syndrome, heart failure leads to increased retention of salt and water by the kidneys. This results in a buildup of fluid in the lungs, causing shortness of breath and fatigue. The body’s response to heart damage is to activate hormonal regulatory systems that attempt to restore normal blood flow to vital organs. Over time, these hormonal systems can lead to secondary damage to the heart and the circulation, resulting in worsening heart failure. Most drugs used to treat heart failure block the harmful effects of high levels of the compensatory hormones.
The study, called the LIFE trial, focused on advanced heart failure patients with reduced pumping capacity, referred to as Heart Failure with a Reduced Ejection Fraction (HFrEF).
“Patients with the most severe heart failure are often not included in clinical trials because they’re so severely ill they don’t qualify to participate,” said first author and Washington University cardiologist Douglas L. Mann, MD, the Tobias and Hortense Lewin Professor of Medicine. “We wanted to study these patients because their condition is so much worse than that of patients with mild or moderate heart failure. It’s basically a different disease. Because medical therapies are limited in these patients, the only treatment options are cardiac transplantation or left ventricular assist devices. Our hope was that treatment with sacubitril/valsartan would prevent the need to transplant patients or use expensive mechanical circulatory assist devices.”
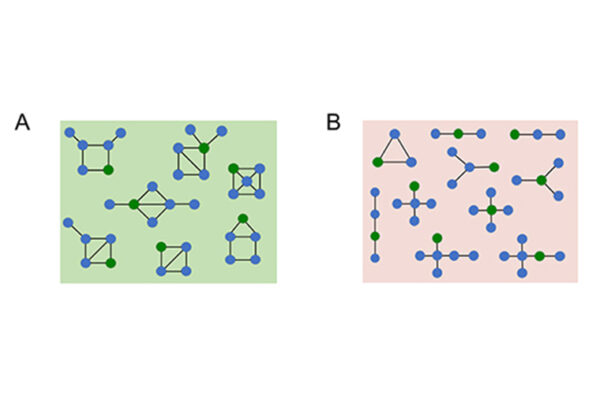
The combination drug sacubitril/valsartan was shown to be more effective than the standard of care — treatment with an angiotensin converting enzyme inhibitor — in a previous large clinical trial involving more than 8,000 heart failure patients with a reduced ejection fraction, but only 60 patients in that trial (less than 1%) had severe disease.
The current LIFE trial included 335 patients with advanced heart failure with a reduced ejection fraction. On average, these patients’ hearts pumped only one-third of the blood volume they should have been pumping. Such patients have chronic shortness of breath and fatigue, even at rest while receiving optimal medical therapy. Half were randomly assigned to receive sacubitril/valsartan along with standard medical therapy for heart failure; the other half received valsartan alone plus standard medical therapy. Neither patients nor researchers knew which patients were in each group. Both drugs are pills taken by mouth. The duration of the study was 24 weeks.
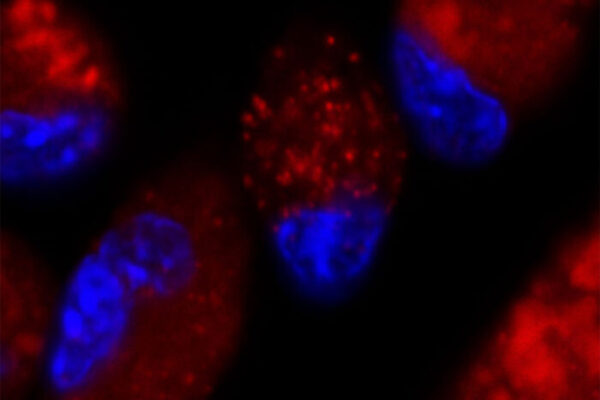
To compare the effectiveness of the drugs, the researchers measured changes in a biomarker that is easily detectable in the blood, called N-terminal pro-Brain Natriuretic Peptide (NT-proBNP). Levels of the biomarker were measured before the patients started treatment and at various times over 24 weeks of therapy. Levels of the biomarker reflect the amount of congestion that heart failure patients have. Decreased levels are associated with improved heart failure symptoms, and increased levels reflect worsening heart failure and increased likelihood of death. The major finding was that there was no statistically significant difference in levels of the biomarker over 24 weeks in the patients taking sacubitril/valsartan, as compared to patients receiving valsartan. This finding was observed across all of the subgroups that were examined.
Compared with valsartan alone, the sacubitril/valsartan treatment group also did not show any improvement in the total number of days alive, days out of the hospital and days that were free from complications of heart failure. Sacubitril/valsartan and valsartan also showed no differences in heart failure hospitalizations, deaths from cardiovascular causes or deaths from any cause. There was a statistically significant increase in potassium levels in the patients receiving sacubitril/valsartan; however, the elevated potassium levels were not life-threatening.
“The findings of the trial were really surprising to us,” said Mann, also a professor of cell biology & physiology. “In every other trial involving sacubitril/valsartan, the drug showed a benefit over the standard of care, including lowering NT-proBNP levels. Even though we didn’t have a large enough sample size in the trial to see clinically meaningful differences in the endpoints between the two groups, every clinical outcome that we measured favored treatment with valsartan alone. Since the results of the trial did not show significant differences in favor of one treatment strategy over the other, we cannot say that valsartan is better than sacubitril/valsartan for patients with advanced heart failure. But as a doctor, I often have to make treatment decisions for my patients based on clinical trial evidence that does not clearly show statistically significant differences between treatment groups. For the most severe heart failure patients, sacubitril/valsartan does not appear to provide an advantage over valsartan, which is a generic drug that is far less expensive to use and was not associated with elevated potassium levels and thus is easier to monitor over time.”
The researchers speculate that the severity of heart failure in the patients in the trial may have resulted in a loss of the beneficial effects of neprilysin inhibition, which would explain why sacubitril/valsartan was no different than valsartan. Experimental and clinical studies have shown that the excessive activation of hormonal systems in severe advanced heart failure can override the drugs that are used to block these systems in order to restore normal balance.
“The evidence suggests that sacubitril/valsartan helps heart failure patients with mild or moderate heart failure but is no better than valsartan for patients with severe disease,” Mann said. “Although we were not able to show a benefit for sacubitril/valsartan in the LIFE trial, we believe that results of the trial will be helpful to the clinicians who provide care for this vulnerable population of advanced heart failure patients. We clearly need to do a better job of preventing heart failure from progressing to an advanced stage, and we need more research to develop better medical therapies for the patients who do progress to advanced stages.”
Lead collaborators on this national clinical trial include researchers at Harvard Medical School and Duke University.
This work was supported by the National Heart, Lung, and Blood Institute (NHLBI) of the National Institutes of Health (NIH), grant numbers U10 HL084904, U10 HL110297, U10 HL110342, U10 HL110309, U10 HL110262, U10 HL110338, U10 HL110312, U10 HL110302, U10 HL110336 and U10 HL110337. Novartis Pharmaceutical Corp. provided the drugs used in the study and partial funding through its investigator-initiated trial program CLCZ696BUS04T.
Mann serves on the steering committee for the PARADISE-MI trial (comparing sacubitril/valsartan to enalapril) for Novartis.
Mann DL, et al for the LIFE Investigators. Effect of treatment with sacubitril/valsartan in patients with advanced heart failure and reduced ejection fraction: a randomized clinical trial. JAMA Cardiology. Nov. 3, 2021.
Washington University School of Medicine’s 1,700 faculty physicians also are the medical staff of Barnes-Jewish and St. Louis Children’s hospitals. The School of Medicine is a leader in medical research, teaching and patient care, consistently ranking among the top medical schools in the nation by U.S. News & World Report. Through its affiliations with Barnes-Jewish and St. Louis Children’s hospitals, the School of Medicine is linked to BJC HealthCare.